Comparative clinicoradiologic research study of the tunnel plastics of multiple gingival recessions with Autograft and Xenogen Collagen matrix
Vedyaeva A.P.1,2*, Brailovskaya T.V.1,2, Tarasenko S.V.1, Bulkina N.V.3, Garibian E.A.1, Nebylitsin I.V.4
1 Moscow State University of Medicine n.a. I.M. Sechenov’s of the Ministry of Health of Russia, 2 Central Research Institute of Dentistry and Maxillofacial Surgery of the Ministry of Health of Russia, 3 Saratov State Medical University n.a V.I. Razumovsky of the Ministry of Health of Russia. 4 Penza State University Medical Institute Faculty of Dentistry, Russia.
ABSTRACT
Aim: To compare the efficacy of gingival recession surgery using a tunnel surgery technique with connective tissue autograft and xenogenic collagen matrix Mucoderm. Material and methods: The article presents the results of a comparative clinicoradiologic analysis of the use of autograft and xenogenic collagen matrix Mucoderm in the tunnel technique of gingival recession treatment. Examination and treatment of 10 patients (6 women, 4 men) aged 35 ± 8.7 years with a diagnosis of generalized gingiva recession, Miller class 2, and with a thin phenotype were performed. Recessions occurred in the area of 49 teeth on the upper and lower jaws. Results: clinical results of root coverage using autograft achieved 99%, and 81% using the xenogeneic collagen matrix Mucoderm. The width of the keratinized attached gingiva for group 1 (autograft) and group 2 (Mucoderm) ranged 0.9 ± 0.44 mm and 1.14 ± 0.2 mm respectively. One month past the surgery with an autograft, it was 4.8 ± 1.1 mm, and by the sixth month it reached a stable value of 3,9 ± 0.8 mm and in comparison, with the values of the group 2 where Mucoderm was used, it was 3.6 ± 0.4 mm and 2.4 ± 0.3 mm respectively. The original thickness of the keratinized attached gingiva of 0.9 ± 0.12 mm, when using connective tissue autografts for the patients’ group 1, increased to 2.4 ± 0.4 mm in a month of the treatment and remained stable by the sixth month being 1.85 ± 0.3mm, as for the patients’ group 2 by the first and sixth months of the treatment it was 2 ± 0.3 mm and 1.5 ± 0.26 mm respectively. Conclusions: The use of the Mucoderm collagen matrix showed statistically significant clinicoradiologic results for class 2 gingival recession coverage for the thin mucous phenotype at long-term dates compared to the “gold standard” of autograft gingival surgery.
Keywords: subepithelial connective tissue graft, mucogingival surgery, keratinized attached gingiva, Mucoderm.
Introduction
Oral health is integral to general well-being [1-3] and relates to the quality of life [4]. Gingival surgery in the recession area is currently a pressing challenge in dental practice, with the disease becoming more prevalent, and given patients’ demands and high esthetic expectations for the results of treatment. Gingival recession is defined as an apical shift of the gingival margin from its physiological position, leading to the exposure of the root surface of the tooth. The gingival recession has complex origins with multiple factors, including both anatomical and drug/treatment-induced factors, and is also associated with such disorders as gingivitis and periodontitis. [5-8] The disease is triggered by topical inflammation that causes the destruction of connective tissue bonding and leads to epithelial proliferation and apical migration, which manifests itself as a gingival recession.
Double-layer techniques of transplanting a connective tissue autograft taken from the hard palate are now the “gold standard” of recession surgery. [9] The indisputable advantages of these techniques are the increase in the keratinized attached gingiva area in the single-stage procedure, the elimination of recessions, gingival thickening (phenotype change), the potential to restore gingival papillae, as well as more predictable and stable treatment results. However, it cannot be ignored that there is a higher rate of surgical injury as a second surgical site is involved. [10]
The microsurgery approach has recently become more common in mucogingival surgery. The tunnel method has been developed for the treatment of gingival recession defects which is technically more complicated but negates the need to make incisions at the base of the gingival papillae and overcomes the anatomical challenges associated with severe resorption of the underlying cortical bone tissue. However, making a conventional partially split mucous flap is fraught with severe complications during the postoperative period, and delivers a poor esthetic result. [11-18]
It is noteworthy that the treatment of recession using the double-layer method is restricted by the size of the autograft, and is associated with a post-surgical hemorrhage risk due to the difficulties of securing reliable hemostasis in the donor area healed by secondary adhesion. [19] These limitations can be overcome by substituting soft gingival tissues for collagen-based materials derived from animals. Mucoderm (Botiss Biomaterials) is one of these alternatives, which contains a non-cross-linked collagen type I and III matrix of porcine origin, which produces a three-dimensional stable matrix and results in a dense structure. Mucoderm ensures revascularization and quick integration of soft tissues and offers an alternative to a connective tissue autograft.
Aim of the study:
To compare the efficacy of gingival recession surgery using a tunnel surgery technique with connective tissue autograft and xenogenic collagen matrix Mucoderm.
Material and methods of the study
Examination and treatment of 10 patients (6 women, 4 men) aged 35 ± 8.7 years with a diagnosis of generalized gingiva recession, Miller class 2, and with a thin phenotype were performed. Recessions occurred in the area of 49 teeth on the upper and lower jaws. The study was conducted according to Good Clinical Practice and the Declaration of Helsinki principles. The study protocol was approved by the Ethics Committees of all participating clinical centers. Informed consent was obtained in writing from all participants before their enrollment in the study.
Criteria for patient eligibility: satisfactory overall health and no contraindications to surgical intervention; the presence of multiple mandibular and maxillary gingival recessions on tooth facial surfaces; keratinized gingiva width (KGW) of 1.5 mm or less; keratinized attached gingiva thickness (KGT) of 1 mm or less; no signs of periodontal inflammation; hygiene index of 2 scores or less.
The gingival recession metrics were measured before the surgical interventions were carried out using a periodontal probe and a needle with a stopper. The following measurements were taken in the middle labial line: 1) recession depth (RD); 2) keratinized gingiva width (KGW); 3) keratinized gingiva thickness (volume) (KGT); 4) dehiscence size in the recession area (DS) using cone-beam computed tomography (CBCT).
The teeth with gingival recessions were classified in the two groups: In total, patients in group 1 had 26 teeth with Miller class 2 recession around 10 incisors, 8 canine teeth and 8 premolars, on which the tunnel method surgical procedure was carried out using an autograft; patients in group 2 had a total of 23 teeth with Miller class 2 recession around 9 incisors, 7 canine teeth and 7 premolars, on which the tunnel method surgical procedure was carried out using the xenogeneic collagen matrix Mucoderm.
All patients had surgical procedures in the gingival recession area using the tunnel surgery technique as recommended by author Otto Zuhr. [17, 18] Under infiltration anesthesia Sol. Articaine hydrochloridi 4%, an epinephrine 1:200000 - 1.7 ml on the labial side were the gingival recession metrics examined. Using a lancet (15С), intrasulcular incisions were made in the recession area, bypassing gingival papillae; then a tunnel micro-raspatory was used to non-invasively reposition the flaps in an apical direction and the region of interproximal surfaces on the gingival papilla base. Then the vertical incisions were made in the alveolar gingiva, muscular fibers were dissected, followed by the deep surgical release of the flap and the creation of the tunnel. The roots of teeth were treated with a zone-specific Gracey curette, periodontal drills, and EDTA 17% gel. A subepithelial connective tissue graft (SCTG) was cut in the palate region, with subsequent hemostasis and wound suturing with Vicryl 3.0. Then the autograft or the xenogeneic collagen matrix Mucoderm was placed into the tunnel formed and stretched to full length using surgical sutures.
The surgery success rate depended on the graft or material stability in the recipient area, and the graft was therefore fixed with encircling stitches (Vicryl 6/0) on the exposed tooth cervical line. Then the apical stabilizing sutures were stitched in the region of alveolar gingiva, with underrunning on the lingual side, and loop sutures, in the region of papillae and vertical incisions (Prolene 5/0). Patients were told to apply cold and observe a bland diet and were prescribed chlorhexidine bi-gluconate 0.12% oral rinse, ibuprofen (200 mg) to be taken three times a day, and amoxicillin (500 mg) to be taken three times a day for one week for the post-surgery period. Sutures were removed on the 14th day after surgery.
The patients’ dental health continued to be carefully monitored for 1 year. The results were quantitatively measured 1, 3, 6 months after the surgical procedure.
The data obtained were statistically processed according to the Mann–Whitney, Wilcoxon test criterion.
Treatment results:
The examination and periodontium status assessment in the patients enrolled in the study revealed 49 teeth with gingival recessions. The metrics varied across the different groups and depending on the gingival phenotype. The deepest recessions were observed around canine teeth (up to 5 mm). The keratinized gingiva width was at its narrowest around incisors and canine teeth (0.5 mm to 1 mm). There was no keratinized gingiva in the region of 11 teeth. The lowest keratinized gingiva thickness was noted in the region of the first and second canine teeth (min. 0.7 mm). The periodontal pockets peaked at 2 mm. On computer imaging, the greatest dehiscence size of cortical bone tissue was observed in the region around the canine teeth, which was recorded at 10.8 mm.
Throughout the study in line with its aim, the comparative analysis of the efficacy of gingival recession surgery was performed using a tunnel surgery technique with autograft and xenogenic collagen matrix Mucoderm.
The need for gingival surgery in the recession area is visible in the following clinical example (Fig. 1-4). Patient N., aged 32, complained of mandibular tooth dehiscence, which she attributed to her ongoing orthodontic treatment. Medical history: surgery of a bifid uvula on the congenital unilateral cleft palate of the maxilla and hard palate on the left side. Miller class 2 recession around teeth 34-44 was visible during the oral examination, the maximum recession depth was 3 mm, the keratinized gingiva width was less than 1.5 mm with a thin gingival phenotype, and the exposed roots of teeth could be visualized and palpated. CBCT showed severe expansive atrophy of the cortical bone tissue on the labial and oral sides, variation in dental root sizes, and those of the mandibular alveolar part (Fig. 1). The following diagnosis was made based on the clinicoradiologic examination: К. 06.0 – generalized gingival recession on the mandible, Miller class 2, thin phenotype. Partially edentulous maxilla. Unilateral cleft hard palate and lip.
The decision was made to correct the gingival recession by applying the tunnel method using a connective tissue autograft around teeth 41-44. The treatment plan was written and communicated to the patient, who gave full informed consent to the treatment (Fig. 1 a-d; Fig. 3).
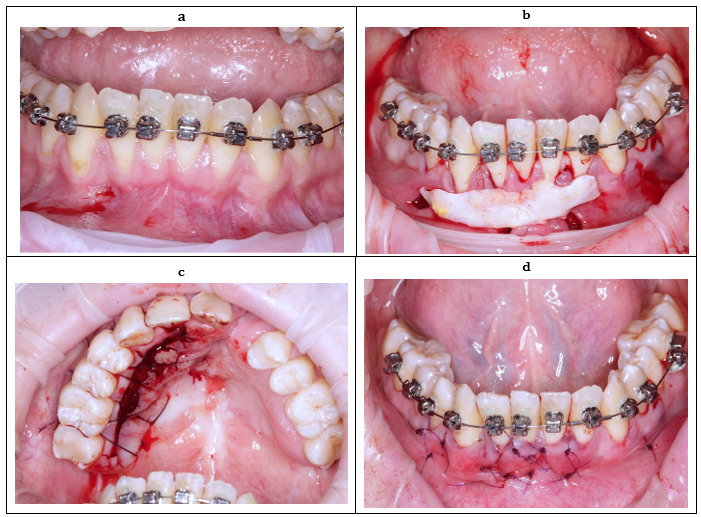
Fig. 1 Patient N., 32. Diagnosis: Miller class 2 generalized gingival recession; а – background: thin phenotype, keratinized gingiva recession, and deficiency around teeth 34-44, b – intrasulcular and apical vertical incisions were made; the tunnel in segment 4 was shaped with micro-raspatories; c – source area of subepithelial connective tissue autograft on the palate; d – the connective tissue autograft was stitched in the recession area.
The subsequent surgery in the region of teeth 31-34 was carried out through the tunnel method using the xenogeneic collagen matrix Mucoderm after 3 months (Fig. 2 а-d; Fig. 4).

Fig. 2. Patient N., 32. а – clinical state after the gingival recession surgery in segment 4 after 6 months, around teeth 32-34, Miller class 2 gingival recession, thin phenotype, keratinized attached gingiva deficiency b – intrasulcular and apical vertical incisions were made, the tunnel in segment 3 was shaped with micro-raspatories c – Mucoderm was injected into the tunnel, stitched in the recession area d – clinical state after the gingival recession surgery in segment 3 after 6 months.
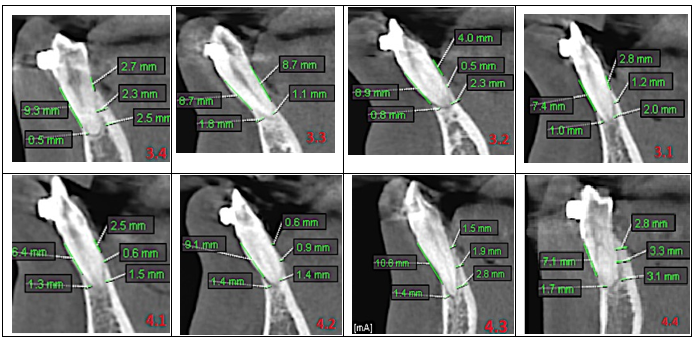
Fig. 3. CBCT series of patient N, 32, pre-surgery. Severe expansive atrophy of the cortical bone tissue was found on the labial and oral sides in the region of teeth 34-44.
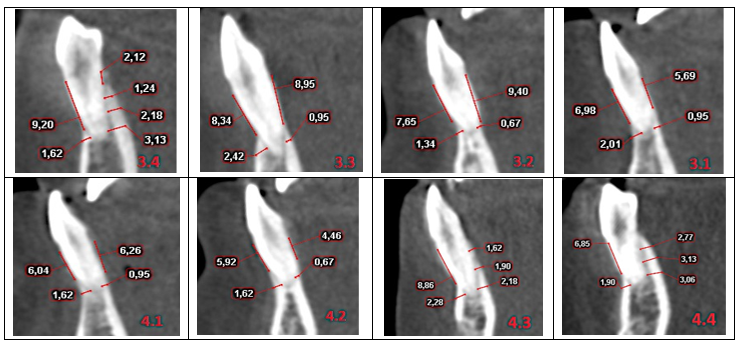
Fig. 4. CBCT series of patient N, 32, 1 year after surgery. An increase was observed in recorded cortical tissue values in the vertical and sagittal planes on the labial side in the region of teeth 34-44.
Discussion
When comparing surgical procedures carried out on Miller class 2 multiple gingival recessions applying the tunnel method using an autograft and those with the xenogeneic collagen matrix Mucoderm, 99% recession coverage of the exposed root surface was achieved using an autograft and 81% using Mucoderm (Table 1). These results differ from the 95% and 91% achieved in the study conducted by Cieślik-Wegemund M. et al. (2016); and the 83% and 53% in the study conducted by Pietruska M. et al. (2018), respectively. Cosgrea R. et al. (2016) and Vincent-Bugnas S. et al. (2017) achieved a 73% and 83% success rate, respectively, when class 2 recessions were covered using the Mucoderm matrix. [20-23]
Group 1 and 2 patients had an initial keratinized gingiva deficiency of 0.9 ± 0.44 mm and 1.14 ± 0.2 mm, respectively. One month after the tunnel method treatment of gingival recession defects using autograft, the average change in keratinized attached gingiva width (KAGW) was 4.8 ± 1.1 mm and stabilized at 3.9 ± 0.8 mm by six months, compared with 3.6 ± 0.4 mm after one month and 2.4 mm ± 0.3 mm after six months in group 2 where Mucoderm was used. Thus, KAGW increased by 3 ± 0.8 mm after applying the autograft, and by 1.3 ± 0.3 mm with the Mucoderm matrix (Table 2). Whereas Cieślik-Wegemund M. et. al. (2016) achieved a 1 mm and 0.8 mm increase; and Pietruska M. et al. (2018) recorded increases of 2.78 mm and 0.52 mm. Cosgrea R. et al. (2016) and Vincent-Bugnas S. et al. (2017) recorded KAGW increases when Mucoderm was used at 0.69 mm and 0.92 ± 0.41 mm, respectively. [20-23]
The patients who underwent tunnel gingival surgery had the recipient's gingival thickness of approx. 0.9 ± 0.12 mm in group 1 (connective tissue autograft) and approx. 1 ± 0.12 mm in group 2 (Mucoderm) (i.e. thin phenotype). With the autograft, the keratinized attached gingiva thickness increased to 2.4 ± 0.4 mm after a month and stabilized at 1.85 ± 0.3 mm after six months, which indicates that the thin periodontal phenotype has been successfully converted into thick gingiva (Biotype switching). After the Mucoderm matrix was applied in group 2, the gingival thickness increased to 2 ± 0.3 mm after one month and 1.5 ± 0.26 mm after six months, which indicates that the thin periodontal phenotype has been converted into a medium-sized one. Thus, the keratinized attached gingiva thickness increased by 0.95 ± 0.36 mm with the autograft and by 0.52 ± 0.3 mm with Mucoderm (Table 3). Whereas in the study conducted by Pietruska M. et. al. (2018), it increased by 1.10 mm and 0.27 mm, respectively. [22]
|
Table 1. Average root surface coverage, mm |
||||||
|
Group |
Pre-surgery |
After 1 month |
After 3 months |
After 6 months |
% coverage |
(p) pre-surgery - 6 months |
|
1 (SCTG) |
2.1 ± 0.7 |
0 |
0 |
0.03 ± 0.07 |
99 |
0.0001 |
|
2 (Mucoderm) |
1.6 ± 0.4 |
0.1 ± 0.2 |
0.3 ± 0.2 |
0.4 ± 0.1 |
81 |
0.0001 |
|
(р) between groups |
- |
- |
- |
- |
0.0001 |
- |
Note: deviations are statistically significant (р <0.05).
|
Table 2. The average change in keratinized attached gingiva width (KAGW), mm |
||||||
|
Group |
Pre-surgery |
After 1 month |
After 3 months |
After 6 months |
KAGW increase |
(p) pre-surgery - 6 months |
|
1 (SCTG) |
0.9 ± 0.44 |
4.8 ± 1.1 |
4.3 ± 1 |
3.9 ± 0.8 |
3 ± 0.8 |
0.0001 |
|
2 (Mucoderm) |
1.14 ± 0.2 |
3.6 ± 0.4 |
3 ± 0.3 |
2.4 ± 0.3 |
1.3 ± 0.3 |
0.0001 |
|
(р) between groups |
- |
- |
- |
- |
0.0001 |
- |
Note: deviations are statistically significant (р <0.05).
|
Table 3. The average change in keratinized attached gingiva thickness (KAG), mm |
||||||
|
Group |
Pre-surgery |
After 1 month |
After 3 months |
After 6 months |
KAG thickness increase |
(p) pre-surgery - 6 months |
|
1 (SCTG) |
0.9 ± 0.12 |
2.4 ± 0.4 |
2.1 ± 0.3 |
1.85 ± 0.3 |
0.95 ± 0.36 |
0.0001 |
|
2 (Mucoderm) |
1 ± 0.12 |
2 ± 0.3 |
1.7 ± 0.3 |
1.5 ± 0.26 |
0.52 ± 0.3 |
0.0001 |
|
(р) between groups |
- |
- |
- |
- |
0.0001 |
- |
Note: deviations are statistically significant (р <0.05).
|
Table 4. The average change in the dehiscence of the outer cortical compact plate, mm |
||||
|
Group |
Pre-surgery |
After 6 months |
Dehiscence decrease |
(p) pre-surgery - 6 months |
|
1 (SCTG) |
7 ± 1.8 |
6.3 ± 1.7 |
0.7 ± 0.27 |
0.002 |
|
2 (Mucoderm) |
5.9 ± 1.4 |
5.8 ± 1.4 |
0.12 ± 0.09 |
0.005 |
|
(р) between groups |
- |
- |
0.0001 |
- |
Statistically significant р <0.05
A minimum volume of blood is supplied to the labial parts of the cortical bone tissue via the periosteum vessels. This means that the bone tissue dehiscence and fenestration on the tooth root facial surface (“hidden recession”) will sooner or later lead to recession and bone defect progression in patients with the thin phenotype. According to computer imaging generated using Planmeca ProMax 3D Mid equipment (35 µSv dose), the pretreatment dehiscence size was 7 ± 1.8 mm in size among the patients from group 1 (connective tissue autograft), and 5.9 ± 1.4 mm among the patients from group 2 (Mucoderm), which is an adverse factor for surgical intervention due to the risk of the autograft or mucous flap necrosis caused by a reduced blood supply to the recipient area. Following gingival surgery applying the tunnel method, an increase in cortical bone tissue of 0.7 ± 0.27 mm was achieved among patients in the autograft group after 6 months, while a 0.12 ± 0.09 mm increase was achieved among those in the Mucoderm group (Table 4). Whereas in the study conducted by Schmitt M. et. al. (2019), it increased by 0.42 ± 0.13 mm and by 0.36 ± 0.18 mm, respectively. [24]
Conclusions
Data from the clinicoradiologic assessment of the autograft and the xenogeneic collagen matrix Mucoderm used in the tunnel surgery technique for coverage of Miller class 2 multiple gingival recessions for the thin phenotype suggests that the use of autograft is preferable. However, the results obtained with the xenogeneic collagen matrix Mucoderm use can also be deemed successful, in terms of both the root coverage (81%), the keratinized attached gingiva width (2.4 ± 0.3 mm) and thin-to-medium phenotype conversion (1.5 ± 0.26 mm), which is sufficient for periodontium tissues to function adequately and for reducing the risk of gingival recession recurring in the future.
Conflict of interests
The author declares no conflict of interest.
References
- Nithya K G, Thangavelu L, Roy A. In Vitro Evaluation of Anticariogenic Activity of Acacia Catechu Extract Against Selected Microbes. Int. J. Pharm. Phytopharm. Res. 2018; 8(3): 64-67.
- Shrihari T G. Beta endorphins – novel holistic therapeutic approach to chronic inflammation associated cancer. Int. J. Pharm. Phytopharm. Res. 2018; 8(5): 35-38.
- Shamsaddin H, Barghi H, Jahanimoghadam F, Farokh Gisour E, Safizadeh S. Prevalence of Dental Pain and Its Relationship with Socioeconomic Status among 6- to 12-Year-Old Children in Kerman, Iran. Arch. Pharma. Pract. 2018; 9(1): 14-20.
- Jahanimoghadam F, Farokh Gisour E, Askari R, Rad M. Attitude Regarding Dental Stem Cells among Dental Practitioners in Kerman, Iran. Arch. Pharma. Pract. 2018; 9(3): 10-13.
- Balandina M.A., Kobozev M.I., Muraev A.A., Ivanov S.Y. The use of connective tissue graft harvested from retromolar area in case of third molar extraction simultaneously with single recession coverage. The Journal of scientific articles “Health and Education Millennium” 2016; 18(1): 107-110. Russian. https://www.elibrary.ru/item.asp?id=25672037.
- Cortellini P., Bissada N.F. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J Periodontol 2018; 89(1): 204-213. https://doi.org/10.1002/JPER.16-0671.
- Pickron R.N. Etiology of gingival recession. Am J Orthod Dentofacial Orthop 2014; 146(6): 693-694. https://doi.org/10.1016/j.ajodo.2014.09.018.
- Zjulkina L.A., Kobrinchuk K.Y., Ivanov P.V., Kapralova G.A. Mechanisms of solution and methods gum recession. Modern problems of science and education 2017; 1: 54-63. Russian. https:// https://www.elibrary.ru/item.asp?id=28401210.
- Zucchelli G., De Sanctis M. The coronally advanced flap for the treatment of multiple recession defects: a modified surgical approach for the upper anterior teeth. J Int Acad Periodontol. 2007; 9(3): 96-103. PMID: 17715841.
- Bespalova N.A., Yanova N.A., Runova N.B., Durnovo E.A. The achievement of soft tissue stability around the teeth and implants. The Russian Bulletin of Dental Implantology.2016;1(33):52-59. https://www.elibrary.ru/item.asp?id=41418723.
- Aroca S., Keglevich T., Nikolidakis D., Gera I., Nagy K., Azzi R. et al. Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol 2010; 37(1): 88-97. https://doi.org/10.1111/j.1600-051X.2009.01492.x.
- Aroca S., Molnar B., Windisch P., Gera I., Salvi G.E., Nikolidakis D. et al. Treatment of multiple adjacent Miller Class I and II gingival recessions with a Modified Coronally Advanced Tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. J Clin Periodontol 2013; 40(7): 713–720. https://doi.org/10.1111/jcpe.121
- Cairo F., Nieri M., Pagliaro U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J Clin Periodontol 2014; 41(15): 44-62. https://doi.org/10.1111/jcpe.12182
- Cortellini P., Pini Prato G. Coronally advanced flap and combination therapy for root coverage. Clinical strategies based on scientific evidence and clinical experience. Periodontology 2000 2012; 59(1): 158-184. https://doi.org/10.1111/j.1600-0757.2011.00434.x.
- Papageorgakopoulos G., Greenwell H., Hill M., Vidal R., Scheetz J.P. Root coverage using acellular dermal matrix and comparing a coronally positioned tunnel to a coronally positioned flap approach. J Periodontol 2008; 79(6): 1022-1030. https://doi.org/10.1902/jop.2008.070546
- Zucchelli G., Marzadori M., Mounssif I., Mazzotti C., Stefanini M. Coronally advanced flap + connective tissue graft techniques for the treatment of deep gingival recession in the lower incisors. A controlled randomized clinical trial. J Clin Periodontol 2014; 41(8): 806-813. https://doi.org/10.1111/jcpe.12269
- Zuhr O., Fickl S., Wachtel H., Bolz W., Hürzeler M.B. Covering of gingival recessions with a modified microsurgical tunnel technique: case report. Int J Periodontics Restorative Dent 2007; 27(5): 457-463. PMID: 17990442.
- Zuhr O., Rebele S.F., Schneider D., Jung R.E., Hürzeler M.B. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: an RCT using 3D digital measuring methods. Part I. Clinical and patient-centered outcomes. J Clin Periodontol 2014; 41(6): 582-592. https://doi.org/10.1111/jcpe.12178.
- Burkhardt R., Hammerle C.H., Lang N.P. Wound Healing. Self-reported pain perception of patients after mucosal graft harvesting in the palatal area. Journal of Clinical Periodontology 2015; 42(3): 281–287. https://doi.org/10.1111/jcpe.12357
- Cieślik-Wegemund M., Wierucka-Mlynarczyk B., Tanasiewicz M., Gilowski L. Tunnel technique with collagen matrix compared with connective tissue graft for treatment of periodontal recession: a randomized clinical trial. J Periodontol 2016; 87(12):1436-1443. https://doi.org/10.1902/jop.2016.150676
- Cosgarea R., Juncar R., Arweiler N., Lascu L., Sculean A. Clinical evaluation of a porcine acellular dermal matrix for the treatment of multiple adjacent class I, II, and III gingival recessions using the modified coronally advanced tunnel technique. Quintessence Int. 2016; 47(9):739-47. https://doi.org/10.3290 / j.qi.a36565
- Pietruska M., Skurska A., Podlewski L., Milewski R., Pietruski J. Clinical evaluation of Miller class I and II recessions treatment with the use of modified coronally advanced tunnel technique with either collagen matrix or subepithelial connective tissue graft: A randomized clinical study. J Clin Periodontol 2019; 46(1):86-95. https://doi.org/10.1111/jcpe.13031
- Vincent-Bugnas S., Borie G., Charbit Y.J. Treatment of multiple maxillary adjacent class I and II gingival recessions with modified coronally advanced tunnel and a new xenogeneic acellular dermal matrix. Esthet Restor Dent. 2018; 30(2):89-95. https://doi.org/10.1111/jerd.12337
- Schmitt C.M., Schlegel K.A., Gammel L., Moest T.J. Gingiva thickening with a porcine collagen matrix in a preclinical dog model: Histological outcomes. Clin Periodontol. 2019; 46(12):1273-1281. https://doi.org/10.1111/jcpe.13196.
Contact Meral
Meral Publications
www.meralpublisher.com
Davutpasa / Zeytinburnu 34087
Istanbul
Turkey
Email: [email protected]