Value of directional enhanced flow and follow up of premature restriction of the fetal foramen ovale
Bejiqi Ramush1-3, Retkoceri Ragip3, Maloku Arlinda3, Mustafa Aferdita3, Bejiqi R. Rinor3, Hana Bejiqi4*
1Texas Health Science Center, University of Texas, San Antonio, Texas, USA. 2Medical School, University of Gjakova “Fehmi Agani”, Gjakova, Kosovo. 3Department of Cardiology, Pediatric Clinic, Medical University of Prishtina, University Clinical Center of Kosovo, Prishtina, Kosovo. 4Medical Faculty, University of Business and Technology, Prishtina, Kosovo.
Correspondence: Hana Bejiqi, Medical Faculty, University of Business and Technology, Prishtina, Kosovo. [email protected]
ABSTRACT
A rare but dangerous disorder that can occur at any point during pregnancy is premature closure or constriction of the foramen ovale. This syndrome can be caused by a variety of defects, either alone or in combination with other congenital and circulatory problems. Arrhythmia, right heart failure, congestion, the hypoplastic left side of the heart, pericardial and pleural effusions, ascites, and nonimmune hydrops can all be seen with early closure of the foramen ovale. Foramen ovale constriction or premature closure, which can be identified by foetal ultrasound during pregnancy, does not have any precise diagnostic criteria. To be diagnosed, a foramen ovale must be at least 2 mm in diameter, have a Doppler velocity of at least 120 cm/s, or be at least 3 mm in diameter with a Doppler velocity-measured gradient of at least 5 mm Hg.
Here, we provide a case of a single foetus at 26 weeks of gestational age with premature closure of the foramen ovale in conjunction with a restrictive atrial septal defect II type throughout the third trimester, follow-up, and normal delivery at the tertiary level of care.
Keywords: Premature closure of foramen ovale, Restrictive foramen ovale, Fetal echocardiography, Hydrops fetalis
Introduction
The term "patent foramen ovale" (PFO) refers to a hole in the heart that did not properly close after birth. A little flap-like opening called a hole exists between the upper heart chambers. The atria are the name for the upper chambers of the heart. It typically closes during infancy. When the foramen ovale doesn't close, it's called a patent foramen ovale.
Vieussens first described this exceedingly rare circulation abnormality, which occurs during intrauterine life, in 1715; an updated version was published in 1875 [1]. The foramen ovale (FO) may close early or become constrained at any point during pregnancy for a variety of reasons. Premature restriction or closure of the FO in structurally normal hearts has been associated with cardiac failure, enlargement of the right ventricle, tricuspid regurgitation, pericardial effusion, and even poor newborn outcomes. There is a dearth of information about these unusual conditions. A rare cardiac anomaly is the premature closure of the foramen ovale. Hepatomegaly, ascites, pleural and pericardial effusions, and widespread edema are all signs of severe right-sided heart failure in these hydropic fetuses. When unexplained fetal hydrops is observed, the differential diagnosis should include premature closure of the foramen ovale [2].
Any time during pregnancy, the foramen ovale might prematurely close or become restricted for a variety of reasons [3].
Foramen ovale (FO) premature closure or constriction is a rare but recognized condition. Several publications have used the parameters FO diameter 2mm and Doppler velocity >120cm/s and diameter 3mm with Doppler velocity measured gradient >5mmHg to define this entity [4].
Case presentation
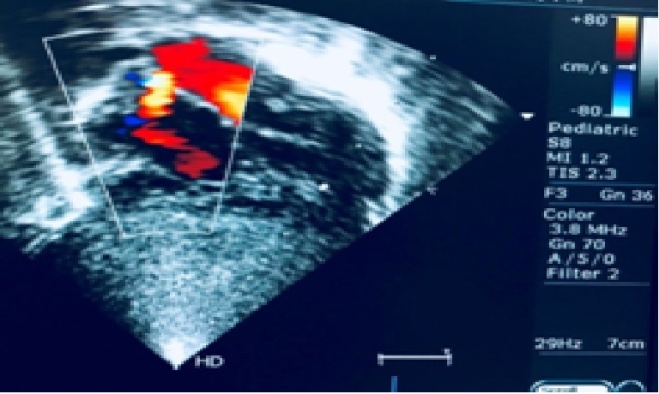
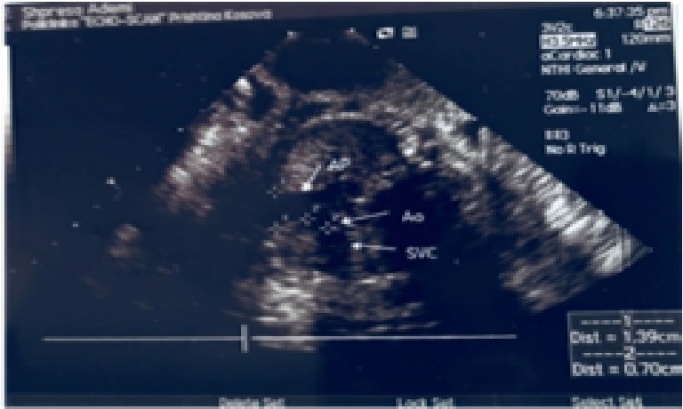
A routine prenatal sonographic test at another institution revealed the presence of asymmetry on the heart sides in a 25-year-old multiparous woman who was carrying her third child and weighed 62 kg (165 cm). The father of the foetus suffered from aortic coarctation and was effectively treated by stenting at age 25. A positive family history of congenital heart disease existed. During the 26 weeks of gestation, we only saw one intrauterine pregnancy. An ultrasound performed during pregnancy revealed a female foetus with a normal growth curve, normal placenta and amniotic fluid index, distinct pericardial effusion, and a normal rhythmic heartbeat. A foetal echocardiogram revealed modest hypoplasia in the left atrium and left ventricle, as well as more than a two-fold increase in the size of the right chambers compared to the left. Using standard colour Doppler imaging, echocardiographic imaging revealed the foetal left foramen ovale bulging without an obvious flap and extremely constrictive flow from the right to the left atrium (Figures 1 and 2). We noticed slower blood flow in the upper portion of the foramen ovale by adjusting the colour scale (from 48 to 24 cm/s); however, red pixels covered the tissues and made it impossible to distinguish the colour signal. There were no further foetal abnormalities found. Additionally, middle holo-systolic regurgitation was seen at the tricuspid valve level with a peak gradient of 23 mmHg. Premature foramen ovale restriction was identified as the diagnosis in our case by echocardiographic testing. At the age of 34 weeks of gestation, using 2D echocardiography we obtained as below measurements data: left ventricle diastolic diameter = 8.6mm, right ventricle diastolic diameter =15.7mm, pulmonary artery =13.9mm, aorta =5.1 – 7.0mm, foramen ovale =2.3-2.8mm, (Figure 4), anterograde flow through the aortic valve was =1.26 - 1.39 m/s (Figure 3).
Despite possible the high risk of complications we suggested continuing pregnancy, with routine echocardiography monitoring and follow-up every week, trying to prolong gestational age as much as possible. Pregnancy was terminated at 38 weeks of gestation by elective cesarean section (both two previous pregnancies were terminated by cesarean section). The male infant was 2780 grams at birth, Apgar score of 7/8. During the first clinical observation, no abnormalities were detected. His cardiac pathology was also confirmed by post-natal echocardiography (Figure 4). The early postnatal period was normal and on the 6th day of life, child was discharged home.
|
|
|
Figure 1. Four chamber view showed small foramen ovale and restrictive atrial septal defect |
|
|
|
Figure 2. Restrictive color Doppler flow through the foramen ovale |
|
|
|
Figure 3. Dimension of the great vessels |
|
|
|
a) |
|
|
|
b) |
|
Figure 4. Note restrictive interatrial communication and hypertrophic right ventricle |
Results and Discussion
First documented by Vieussens in 1715 and then again in 1875, premature closure or constriction of the foramen ovale is an extremely uncommon cardiovascular defect that happens during intrauterine life [1].
Incidence Although extremely rare, premature foramen ovale closure does occur occasionally. According to the autopsy , congenital cardiac disease accounts for around 90:10.000 neonatal fatalities and 60:10.000 neonatal deaths overall. Ten times fewer people have the solitary form than the related forms [2].
Etiology Numerous cardiac defects, left hypoplastic hearts, and left blockages can be causes or outcomes of premature closure of the foramen ovale. The left hypoplastic heart is believed to be an early cause or consequence, whereas obstructive processes are supposed to be a late cause, resulting in left-side heart enlargement [3].
The foramen ovale can prematurely close on its own or in conjunction with other congenital and circulatory conditions. Arrhythmia, pericardial effusion, pleural effusion, ascites, and nonimmune hydrops can all be associated with premature closure of the foramen ovale, right heart failure, and congestion [4]. Using foetal echocardiography, it is possible to assess the foramen ovale and determine whether it is prematurely closing or narrowing. Foramen ovales can be identified when their diameter is less than 3 mm and their Doppler velocity-measured gradient is larger than 5 mm Hg, or when their diameter is less than 2 mm and their Doppler velocity-measured gradient is greater than 120 cm/s [5]. Because it's possible that the fossa ovalis will remain open even when the foramen ovale is closed or narrowed, diagnosing an atrial septal aneurysm may be more challenging. In both of our cases, the Doppler velocity is frequently obscured by the absence of a blood flow signal. The use of colour Doppler imaging is restricted to the diagnosis of this condition. To detect whether the blood pressure is abnormally high or abnormally low, a doppler is required. It is challenging to see low-velocity blood flow through the foramen ovale on typical colour flow maps [6].
When a foetus' foramen ovale has prematurely closed or is otherwise restricted, the timing of delivery is extremely important. Foramen ovale constriction is present in our case during the third trimester of the patient's foetus. Pregnant women and obstetricians can decide on the timing of birth with the use of a follow-up foetal echocardiogram [7]. Identification of early foramen ovale closure or constriction requires close observation of the foetus's vital signs. Early foramen ovale closure during pregnancy has been linked to severe left ventricular hypoplasia and perhaps even embryonic mortality. Because of the restricted blood flow, a very early foramen ovale closure during pregnancy may induce a hypoplastic left heart with an aneurysm that ruptures into the left atrium. However, right heart failure has been linked to delayed closure more commonly than the development of an atrial septal aneurysm [8].
Aneurysms that bulge into the right atrium can be the result of a left-sided obstructive disease. The left-sided chambers in these patients are only slightly smaller in size, which may suggest that the foramen ovale was closed later [9]. These patients also have a substantial septal aneurysm. A small foramen ovale, such as the one in our case, may offer an additional blood flow route to the left atrium. Foramen ovale premature closure is particularly risky for foetuses, as it may result in pulmonary vascular dysfunction and subsequently persistent pulmonary hypertension [10].
As was already indicated, the directional display resolves the trade-off between aliasing and the high detectability of low-velocity flow. We discovered right-to-left atrial flow in our patient using DeFLOW technology [11]. Our observation of flow from the right to left atrium abundantly supports the diagnosis of a foramen ovale constriction. When determining whether to continue the pregnancy or discontinue it, as well as for effective postnatal care and follow-up, this is essential.
Using a composite pulse emission approach and a shorter pulse length, D'eFLOW delivers high spatial and temporal resolution and more accurately depicts capillary perfusion and blood flow continuity. This promise was proven in our case by D'eFLOW's sensitive and precise detection of premature foramen ovale closure or constriction.
The septum primum comes in opposition to the septum secundum and its foramen ovale, closing the communication between the foramen ovale and the ostium secundum (right atrium and left atrium) in this specific case of isolation and restriction of the foramen ovale at term, which is likely the result of an early "physiological" process (that, in our opinion, ends up not being physiologic) [6, 8]. The ultrasonography results suggested a moderately pathogenic disease in the range of findings typically seen in conditions similar to the one for which they were obtained, and it was determined that they matched a recent event. Ultrasonography frequently reveals pericardial effusion, right heart enlargement with left septal wall bulging, and lack of the foramen ovale's flap with left wall bulging in late premature closures or constriction of the foramen ovale [5]. Fortunately, in our case, the only problems we found were a healthy foetus, holosystolic tricuspid regurgitation, and initial right ventricular enlargement. The foetal heart's short route for oxygenating the organs, the brain, and the heart itself is known as the foramen ovale. When foetal movements and oxygen intake decrease, foetal hypoxia and heart failure are prevented, at least temporarily.
Conclusion
This case study shows a potentially uncommon instance of a foetus with a prematurely closed foramen ovale in conjunction with a restrictive atrial septal defect, which results in almost normal foetal circulation, the foetus's survival to term, and a successful delivery. Our case is a rare instance of early diagnosis of premature constriction of the foramen ovale in a foetus with normal cardiac morphology and a normal foetus growing and developing, to the author's knowledge.
Acknowledgments: The family that participated in this study is acknowledged by the authors for their cooperation.
Conflict of interest: None
Financial support: None
Ethics statement: The Institutional Review Board at our Clinical Centre gave its blessing to this report, and both parents signed written informed permission forms.
Consent For the purpose of publishing this case report and any related photos, the patient's parents' written informed consent was acquired.
References
- Sierra JM, Jeanty MP, Tzachrista PE. Premature closure of the foramen ovale. The Fetus.net. 2002;19(11):105.
- Coulson CC, Kuller JA. Nonimmune hydrops fetalis secondary to premature closure of the foramen ovale. Am J Perinatol. 1994;11(6):439-40.
- Pernot C, Marchal C, Ravault MC, Cloez JL, Lambert A. Premature closure of the foramen ovale. Arch Fr Pediatr. 1979;36(9):949-58.
- Li YD, Li ZA, He YH. Premature closure or restriction of the foramen ovale: prenatal diagnosis by directional enhanced flow imaging. J Ultrasound Med. 2013;32(7):1291-4. doi:10.7863/ultra.32.7.1291
- Gupta U, Abdulla RI, Bokowski J. Benign outcome of pulmonary hypertension in neonates with a restrictive patent foramen ovale versus result for neonates with an unrestrictive patent foramen ovale. Pediatr Cardiol. 2011;32:972-6.
- Bellotti M, Bruzzese P, Riparini J, Rognoni GC, Marconi A, Autuori M. First trimester cardiac parameters in the early screening of congenital heart disease (CHD) using high resolution flow imaging mode (e-flow). Ultrasound Obstet Gynecol. 2012;40(suppl):90.
- Iwamoto Y, Tamai A, Kawasaki H, Taketazu M, Senzaki H. Late clinical manifestations of mitral valve disease and severe pulmonary hypertension in a patient diagnosed with premature closure of foramen ovale during fetal life. World J Pediatr. 2011;7:182-4.
- Nowlen TT, Ayres NA, Kearney DL, Nihill MR, Grifka RG. Premature closure of the foramen ovale associated with aortic stenosis, left ventricular dilation with thrombus, and early mortality. Am J Cardiol. 2000;85(9):1159-61.
- Chrysostomou C, Romaguera RL, Rodriguez MM. Giant aneurysm of the atrial septum associated with premature closure of foramen ovale. Cardiovasc Ultrasound. 2005;3(1):20.
- Stanek J, Bove KE, Bofinger M. Premature closure of foramen ovale and renal vein thrombosis in a stillborn twin homozygous for methylene tetrahydrofolate reductase gene polymorphism: a clinicopathologic case study. J Perinat Med. 2000;28:61-8.
- Dong FQ, Zhang YH, Li ZA, Hou ZZ, He XJ, Guo YZ. Evaluation of normal fetal pulmonary veins from the early second trimester by enhanced-flow (e-flow) imaging echocardiography. Ultrasound Obstet Gynecol. 2011;38(6):652-7.
Contact SPER Publications
SPER Publications and
Solutions Pvt. Ltd.
HD - 236,
Near The Shri Ram Millenium School,
Sector 135,
Noida-Greater Noida Expressway,
Noida-201301 [Delhi-NCR] India