Ultrasonographic changes of abdominal subcutaneous fat after different noninvasive treatment methods in women with central obesity
Hisham A. Al-waseif1*, Nebal A. R. Aboul Ella2, Samah M. Ismail3
1Radio and TV Union Medical Care, Egypt.2Professor of Pediatrics and Clinical Nutrition Consultant, National Nutrition Institute, General Organization of Teaching Hospitals and Institutes. Egypt. 3Assistant Professor of Physical Therapy for Cardiovascular/Respiratory Disorder and Geriatrics, Faculty of Physical Therapy, Cairo University, Egypt.
ABSTRACT
Background: Central obesity is a common associating problem in obese women, which leads to various diseases as it is related to a higher risk of hypertension, insulin resistance, heart disease, and type 2 diabetes mellitus. Objective: To determine the efficacy of cryolipolysis on abdominal subcutaneous fat in women with central obesity. Material and Methods: Sixty women with central obesity with the age ranged from 35-45 participated in this study at Radio and TV Union Medical Care. They were randomly assigned into three equal groups: Group (I) consisted of 20 women who received low caloric diet (around 1200 kcal) and cryolipolysis therapy. Group (II) consisted of 20 women who received low caloric diet (around 1200 kcal) and abdominal exercises. Group (III) consisted of 20 women who received low caloric diet (around 1200 kcal) with cryolipolysis therapy and abdominal exercises. The study period was 12 weeks. Waist circumference (WC), waist-hip ratio (WHR), body weight, body mass index, and ultrasonographic changes of abdominal subcutaneous fat were evaluated before and after the study. Results: There was a significant decrease in waist circumference, body weight, waist-hip ratio, body mass index, and abdominal fat thickness in all three groups. On comparing the results of the groups after treatment, there were significant differences in abdominal fat thickness, WHR, and WC between groups (I) and (II). Moreover, there were significant differences in WC, WHR, and abdominal fat thickness between groups III and I; and finally, there were significant differences in WC, WHR, and abdominal fat thickness between groups III and II. Conclusion: It can be concluded from the results of this study that cryolipolysis was more effective in reducing abdominal adiposity when applied along with abdominal exercises and diet control in women compared to when it was used alone.
Keywords: central obesity, cryolipolysis, abdominal exercises.
Introduction
Obesity is a medical condition by the accumulation of fat, which is tending to cause damage for health. [1, 2] Energy-rich food intake, bodily inactivity, and genetic susceptibility are the main causes of obesity. [3] Obesity is one of the causes of death and is increasing worldwide. [4, 5] Among the 20 most populouscountries, the highest rate of overweight in young adults and children is in the US (about 13%). Egypt tops the list of adult obesity rates, with about 35% (About 19 million Egyptian) overweight people. [6] In addition, obesity pestilence is quickly increasing in developing countries. [7]
Moreover, central obesity is related to the elevated grads of fat. These results show that the party from having control over metabolic involvements like insulin resistance, diabetics and elevate cholesterol. Furthermore, the lowering of visceral fat regularly decreases the danger of cardiovascular disease. [8, 9]
Central obesity is an ingredient of metabolic syndrome that plays an important role in the development of chronic heart diseases and some cancers by activating mediating agents of diabetics, dyslipidemia, systematic inflammation, etc. even among persons with normal weight. [10] This danger increases by growing abdominal fat. [11]
If body mass index (BMI) i.e. dividing one's weight by the square of his/her height, is 25-29.9 kg/m2, he/she is considered overweight [12] and when it exceeds 30 kg/m2 he/she is considered obese.
Bodyweight stays the same when the calorie intake is similar to calorie consumption. Through time, when people take extra calories than they burn, the energy balance seeks to weight increase. More agents that can lead to energy imbalances and weight gain include genes, where and how people live, eating habits, emotions and attitudes, income, and life habits. [13]
Obesity treatment begins with lifestyle administration (diet, physicalactivity, and behavior modification), which include self-observation of caloric intake and physical activity, goal setting, and retrogression protection. [14]
Behavioral modification, diet, and exercise should be considered in obesity management. Other tools like pharmacotherapy for BMI of 27 kg/m2 or increase with comorbidity or BMI above 30 kg/m2, bariatric surgery for BMI of 35 kg/m2 with comorbidity or BMI above 40 kg/m2 should be utilized in behavioral modification for lowering consumed food and increase physical activity if possible. [15]
Cryolipolysis is a technique utilized to damage fat cells by freezing. The first role is the controlled use of cooling, at the temperatures from +5 to −5 °C, to reduce non-invasive localized fat deposits, resulting in bodyreshaping. Exposure to cooling may cause apoptosis (programmed cell death) of subcutaneous fat tissue, without any clear harm to the overlying skin. [16]
Abdominal muscle practice exercise has been recognized to excess the force and endurance of the abdominal muscles and reduce the size of abdominal subcutaneous fat cells. In a study, moderate 20-week exercise reduced the cell size around 18% in 45 obese women; diet alone did not influence the cell size. [17]
Liposuction clinical investigations have shown 21.7% small complications and 0.38% major complications. [18] Likewise, the incidence of great wound complications was 6.3%, and the great morbidity incidence was 6.8% during thirty days after the surgical procedure of body contouring. [19]
Patients and Methodology
- Patients
Sixty women with central obesity and age range from 35 to 45 were selected from Radio and TV union medical Care, Cairo, Egypt. The study was conducted in Physical Therapy out Patients Clinic of Radio and TV union medical care, Cairo, Egypt, during a period from June 2016 to March 2017.
All patients received a complete explanation of the objectives and procedures of the study. They received and learned the exchange list of food and written informed consent was signed by each patient before participation in the study. Before starting the program, a complete history and physical examination were taken from all patients with particular attention paid to identify any long-term complications of obesity. The Ethics Committee of Faculty of Physical Therapy, Cairo University, Egypt (P.T.REC/012/001151) was reviewed and approved this study.
Patients were chosen under the following criteria: Sixty obese women with central obesity, their age range was 35-45 years. Their waist circumference was >90 cm and their waist-hip ratio was >0.85. They were randomly assigned to three equal groups (I, II, & III).
Patients with one of the following criteria were excluded from the study: chronic respiratory disorders, cardiovascular problems, diabetic patients, presence of skin diseases in abdominal regions that prevent the use of cryolipolysis therapy, women with kidney or liver disease, women with any back dysfunctions that prevent them make abdominal exercises, women engaged in another program of exercise training.
- Instrumentations:
- Evaluative equipment and tools:
- Standard weight and height scale (TAY-20-RT) was used to measure the weight and height of each woman.
- Tape measurement (Fiber Glass Tape, China): It was used to measure the waist and hip circumferences to calculate the waist-hip ratio for each woman in the study.
- Food frequency questionnaire: All women in the study were given a list of around 100 food items indicating their intake (frequency and quantity) per day, week, and month.
- Ultrasound imaging device (Medson, Korea, 5–13 MHz): It was used to measure the abdominal subcutaneous fat thickness.
- Treatment equipment and tools:
- Cryolipolysis device (3-max cool shaping, Korea).
- Low-calorie diet (around 1200 kcal) list. For diet control
Procedures:
Assessment procedures:
Assessment of each woman in the three groups before and after the study was performed as follows:
- Weight and height measurements
Weight and height of each woman were measured using weight and height scale and then BMI for each woman was calculated using the following formula: BMI= weight (kg)/height (m2). [20]
- Waist and hip circumference measurements:
At the end of gentle expiration, waist circumference was measured at the level between the iliac crest and the costal margin. The hip circumference was measured at the widest level over the buttocks with the female in standing position. Then the waist/hip ratio was calculated for each woman by dividing the waist circumference by the hip circumference. [21]
- Ultrasound imaging:
Subcutaneous adipose tissue (SAT) thickness was assessed using B-mode ultrasound (Medson, Korea, 5–13MHz). For the assessment, women were placed in the supine position with buttocks, heels, and shoulders in contact with the bed. The thickness of subcutaneous fat was measured by the placement of a 7.5-MHz probe using gel perpendicular to the skin positioned 2 cm above, below, right, and left to the umbilical scar without pressure on the abdomen in order not to distort the measurement. Each of the measurement locations were marked with ink on the skin in order to standardize the transducer position. Longitudinal scans were obtained along the middle line (linea alba). The subcutaneous fat thickness is the distance between the skin–fat barrier andthe anterior surface of the linea alba. [19] Example of sonographic measurements of women in group III in this study is shown in figures (1) and (2).
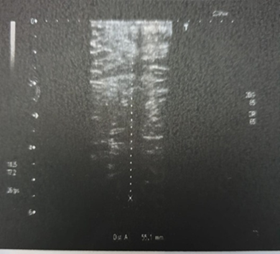
Fig (1) subcutaneous fat thickness pre-study
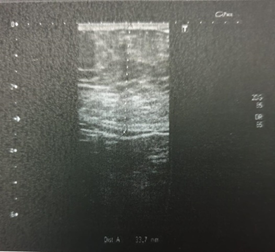
Fig (2) subcutaneous fat thickness post-study
- Dietary assessment:
- 24 Hours Dietary Recall:
All women in the study were asked to recall all food and drink taken in the previous 24 hours.
- Dietary history:
All women in the study were asked for details about intake, types, amount, frequency, and timing needs to obtain.
Treatment procedures:
- Each woman in all groups received a diet plan list around 1200 kcal and learned about the uses of the exchange list and food calories tables. Each woman in groups (I) and (III) was given instructions about the treatment procedures and the benefits of cryolipolysis and each woman in groups (II) and (III) was given instructions about the abdominal exercises.
The procedure of cryolipolysis:
- Each woman in groups (I) and (III) were told to stay in a supine position with the abdominal area uncovered for application of cryolipolysis device.
- Abdominal area divided into 4 zones according to the size of the cryolipolysis cup.
- Each zone was covered by cryolipolysis sheet to prevent skin burn and put the cup on each zone.
- A vacuum was applied through this cup applicator, which ultimately sucked in the treated roll of fat. The patient felt a firm pulling sensation during this action. In the first ten minutes, the temperature within the cup was gradually lowered until it reached a predetermined temperature of about -5 or -6 °C, thereby slowly freezing the fat cells within the roll of fat. The cup applicator stayed in contact with the treated roll of fatthrough the suction process for 30min, each area, treated with any single cup applicator required 45 minutes of cooling per zone with a total of three hours for the whole abdominal area, each woman received one session every 4 weeks for 3 months (a total of three sessions).
The procedure of abdominal exercises:
The women started the abdominal crunch exercise from the resting position and were instructed to raise their shoulders and head upward until their shoulder blades cleared the table. The proper performance of the two exercises was verbally explained to the participants before the procedure began. All participants were instructed on how to perform abdominal exercises according to procedures described by Richardson et al.[22]Every contraction was held for 3 to 5 seconds, with a resting time of 6 to 10 seconds between each repetition. [23]
Abdominal crunch:
Lying on the back, knees bent, hands pointed to knees and legsflat on the bed, shoulders were raised until touching the kneecaps with fingers and then returned to the starting position for 1 repetition. [24]
Cross crunch:
Lying supine with knees bent and feet on bed and hands pointed to the knees then lift and rotate hands over to opposite knee. This procedure was repeated ten times and after that, the same procedure was done on the opposite side (knee) for 1 set.[25]
Each woman in the groups (II) and (III) participated in abdominal crunch exercises (abdominal crunch and cross crunch) 10 repetitions in 1 set for 3 sets (10×3) for each type of crunch exercise, 3 times/week for 12 weeks.
Statistical procedures:
In this study, the mean, the standard deviation, and the standard error were calculated for each group in the study. The mean, the standard deviation were used as a primary source of connecting facts about each parameter to measure central tendency.
Paired t-test was used to compare within each group and to detect the level of significance in each group. ANOVA was used to detect significance level between the two groups (comparison). The SPSS software was utilized for data analysis and the level of significance was set at 0.05 level.
Results
This study was carried out to determine the impact of different noninvasive treatment methods on abdominal subcutaneous fat in women with central obesity. Comparing the common properties of the topics of the three groups showed that there was no considerable variation among the three groups in the mean age, weight, height, BMI, waist circumference (WC) or waist-hip ratio (W/H) (p > 0.05) as reported in Table (1).
The results showed that there was a considerable reduction in superior abdominal fat thickness by 24.23%, 12.39%, and 35.89% in groups I, II, & III, respectively; inferior abdominal fat thickness by 23.65%, 12.39%, and 34.73% in groups I, II, & III, respectively ; right abdominal fat thickness by 27.54%, 13.28%, and 40.93% in groups I, II, & III respectively; left abdominal fat thickness by 27.11%, 12.38%, and 41.72% in groups I, II, & III, respectively; waist circumference by 10.37%, 4.96%, and 15.04% in groups I, II, & III respectively and W/H ratio by 4.8%, 1.9%, and 11.42% in groups I, II, & III, respectively. On post-treatment comparing the results of the 3 groups, there were significant differences in abdominal fat thickness, WHR, WC and between groups (I) and (II); significant differences in abdominal fat thickness, WHR, and WC between groups (III) and (I); and finally there were significant differences in WC, WHR, and abdominal fat thickness in groups (III) and (II) (Table (2)).
|
Table 1. Descriptive statistics and ANOVA test for the mean age, weight, height, and BMI of the three groups (Groups I, II, and III). |
|||||
|
|
Group I |
Group II |
Group III |
p-value |
Sig |
|
|
|
|
|||
|
Age (years) |
40.6 ± 3.42 |
40 ± 3.69 |
41.15 ± 3.77 |
0.6 |
NS |
|
Weight (kg) |
86.05 ± 4.77 |
87.1 ± 4.94 |
85.4 ± 4.97 |
0.54 |
NS |
|
Height (cm) |
165.05 ± 3.67 |
165.1 ± 3.69 |
164.3 ± 3.94 |
0.75 |
NS |
|
BMI (kg/m²) |
31.71 ± 1.43 |
32.54 ± 2.69 |
32.21 ± 2.81 |
0.55 |
NS |
|
WC (CM) |
111.85 ± 6.76 |
109.75 ± 5.6 |
112.65 ± 5.63 |
0.29 |
NS |
|
W/H ratio |
1.04 ± 0.03 |
1.05 ± 0.03 |
1.05 ± 0.01 |
0.68 |
NS |
|
|
SD: Standard deviation, |
p value: Probability value, |
NS: Non significant |
- Results of the pre- and post-treatment mean values of WC, W/H ratio, and abdominal fat thickness of the three study groups pre and post the study: as shown in Table (2)
|
Table 2: Mean values and standard deviations of anthropometrics and sonographic measurements before and after the treatment in the three groups. |
|
||||||
|
Groups |
Pre-study Mean±SD |
Post-study Mean±SD |
p-value |
% of improvement |
|
||
|
Waist circumference (CM) |
I |
111.85 ± 6.76 |
100.25 ± 6.88 |
0.0001* |
10.37% |
|
|
|
II |
109.75 ± 5.6 |
104.3 ± 5.49 |
0.0001* |
4.96% |
|
||
|
III |
112.65 ± 5.63 |
95.7 ± 5.01 |
0.0001* |
15.04% |
|
||
|
p-value |
0.75** |
0.0001* |
|
||||
|
f-value |
0.28 |
15.55 |
|
||||
|
W/H ratio |
I |
1.04 ± 0.03 |
0.99 ± 0.02 |
0.0001* |
4.8% |
|
|
|
II |
1.05 ± 0.03 |
1.03 ± 0.04 |
0.0001* |
1.9% |
|
||
|
III |
1.05 ± 0.01 |
0.93 ± 0.01 |
0.0001* |
11.42% |
|
||
|
Among groups |
p-value |
0.68** |
0.0001* |
|
|||
|
f-value |
0.38 |
71.13 |
|
||||
|
Superior abdominal fat thickness (cm) |
I |
4.91 ± 0.66 |
3.72 ± 0.66 |
p = 0.0001* |
24.23% |
|
|
|
II |
4.76 ± 0.63 |
4.17 ± 0.56 |
0.0001* |
18.12% |
|
||
|
III |
4.82 ± 0.61 |
3.09 ± 0.61 |
0.0001* |
35.89% |
|
||
|
Among groups |
p-value |
0.75** |
0.0001* |
|
|||
|
f-value |
0.28 |
15.55 |
|
||||
|
Inferior abdominal fat thickness (cm) |
I |
5.03 ± 0.64 |
3.84 ± 0.71 |
p = 0.0001* |
23.65% |
|
|
|
II |
4.92 ± 0.61 |
4.31 ± 0.57 |
0.0001* |
20.39% |
|
||
|
III |
4.98 ± 0.61 |
3.25 ± 0.61 |
0.0001* |
34.73% |
|
||
|
Among groups |
p-value |
0.85** |
0.0001* |
|
|||
|
f-value |
0.15 |
13.73 |
|
||||
|
Right abdominal fat thickness (cm) |
I |
4.61 ± 0.54 |
3.34 ± 0.58 |
0.0001* |
27.54% |
|
|
|
II |
4.29 ± 0.54 |
3.72 ± 0.57 |
0.0001* |
13.28% |
|
||
|
III |
4.47 ± 0.59 |
2.64 ± 0.56 |
0.0001* |
34.94% |
|
||
|
Among groups |
p-value |
0.19** |
0.0001* |
|
|||
|
f-value |
1.68 |
18.08 |
|
||||
|
Left abdominal fat thickness (cm) |
I |
4.61 ± 0.54 |
3.36 ± 0.58 |
0.0001* |
27.11% |
|
|
|
II |
4.28 ± 0.54 |
3.75 ± 0.55 |
0.0001* |
12.24% |
|
||
|
III |
4.41 ± 0.63 |
2.57 ± 0.63 |
0.0001* |
41.72% |
|
||
|
Among groups |
p-value |
0.19** |
0.0001* |
|
|||
|
f-value |
1.68 |
20.54 |
|
||||
|
|
|
|
|
||||
SD: Standard Deviation, ↑: increase, t-value: unpaired t value, P-value: Probability Level, **: Nonsignificant, *: Significant
Discussion
Abdominal obesity is the excess levels of visceral fat and has been known as a significant risk factor for metabolic syndrome, T2DM, and CVD. [26]
Waist circumference (WC) measurement is an appropriate method for estimating the degree of central fat distribution. This method has been confirmed as a very beneficial method for estimating those at high risk of ‘metabolic complications’ of obesity and estimated health problems as an outcome of weight gain in the abdomen. [27]
Cryolipolysis is a novel and promising step to reduce nonsurgical fat and body contouring and an alternative to invasive methods such as liposuction. This procedure dramatically reduces fat when used in localized adiposities. This mechanism was performed by using an applicator in the purposed region at a specific cooling temperature that targets adipocytes while sparing the skin, vessels, nerves, and muscles. [28]
The objective of this research was to investigate the effect of different noninvasive treatment methods on abdominal subcutaneous fat in women with central obesity. Sixty sedentary obese women with central obesity, aged from 35-45 years were included in this research. They were randomly divided into three groups: Group (I) consisted of 20 women, receiving a low-calorie diet (about 1200 kcal) and cryolipolysis treatment. Group (II) included 20 women. They received abdominal exercises and a diet with a low calorie (about 1200 kcal). Group (III) included20 women, who received a low-calorie diet (about 1200 kcal) with cryolipolysis therapy and abdominal exercises. The study period was 12 weeks.
Analysis of the results of the present study revealed that the combination of cryolipolysis therapy, diet, and abdominal exercises (group III) had the most positive effect (reduction) in WC, W/H ratio, and abdominal subcutaneous fat as WC and W/H ratio decreased by 15.04% and 11.42%, respectively and superior, inferior, right, and left abdominal fat thickness decreased by 35.89%, 34.73%, 40.93%, and 41.72%, respectively, while in group (I), WC and W/H ratio decreased by 10.37% and 4.8%, respectively and the superior, inferior, right, and left abdominal fat thickness decreased by 24.23%, 23.65%, 27.54%, and 27.11%, respectively. In group II, WC and W/H ratio decreased by 4.96% and 1.9%, respectively and superior, inferior, right, and left abdominal fat thickness decreased by 12.39%, 12.39%, 13.28%, and 12.38%, respectively.
The results of the current study are supported by the results of Krueger, who reported in his clinical studies that after one treatment session, cryolipolysis reduced subcutaneous fat at the treatment site by up to 25%. Advancement was seen in 86% of treated objects. The patient satisfaction is higher than with other techniques used for non-invasive lipolysis. [29]
Ferraro et al., 2012 [30]reported that there was a considerable reduction in the waist circumference with an average decrease of 4.45 cm by the end of the treatment duration. Moreover, initial human and animal investigations have shown a 20-80% reduction in the superficial fat layer thickness, after a single cryolipolysis treatment. [31]Findings from the clinical studies have demonstrated the efficacy and safety of cryolipolysis in humans. [32]
Other previous studies found that fat cells are more susceptible to cold than other types of cells and that controlled cold exposure of adipocytes lead to apoptosis and the resultant death of fat cells without affecting surrounding structures. [33]
Zelickson et al., 2015 [34] carried out research with 42 patients who were subjected to a single usage of cryolipolysis in the thigh area. They observed a considerable decrease in the fat layer during circumference measurement and ultrasound images 16 weeks after therapy. Meanwhile, its technique is not fully to comprehend, it is approved that vacuum suction with adjusted heat extraction prevents blood flow and influencing crystallization of the targeted adipose tissue upon completion of cryolipolysis. [35]
Another mechanism suggests that the initial cold ischemic injury and the injury of crystallization induced by cryolipolysis is enhanced by ischemia-reperfusion injury, leading to the generation of reactive oxygen species, activation of apoptotic pathways, and increase of cytosolic calcium levels. Finally, cold ischemic and crystallization injury of the targeted adipocytes lead to apoptosis of the cells and a noticeableinflammatory response, leading to their removal from the treatment site after several weeks. [16]
There is supportive proof that intracellular “lipid ice” consists at about 10.0°C (than with water ice at 0 °C). The presence of lipid ice may be participating in the occurring death or late apoptosis of fat cells. Through cold ischemic damage, other recognized techniques that elevate cell death are concerning to disturbances in osmoregulation (cell edema), lowering Na-K-ATPase activity and adenosine triphosphate levels, and intracellular lactic acidosis. [36]
Dover et al., 2009 [37] estimated that the utilize of cryolipolysis for the fat level lowering of the flanks (love handles) and back (back fat pads). Pre-programmed therapy was utilized to control the ratio of heat and period therapy. A contralateral, untreated region preserved. The temporary outcomes showed that from 32 topics, the performance is estimated by three performance mechanisms: ultrasound measurement of fat layer lowering than with pre-treatment and post-treatment. The results showed that the ultrasound measurements possessed on a subset of 10 topics explained a fat layer lowering in 100% of these topics with an intermediate lowering of 22.4% at 4 months post-therapy. Safety of the cryolipolysis procedure was also explained with these temporary results as there were no device-related retrograde events reported.
Carruthers et al., 2014[38] illustrated that the cryolipolysis may promote neocollagenesis by extension of the fibroblasts. Other than for the appropriate surface applicator, most cryolipolysis therapy is delivered utilizing vacuum applicators. The vacuum suctions that withdrawal the tissue bulge into the therapy cup may supply moderate extension to the skin and contribute to neocollagenesis.
The results of an investigation [16] showed that there was a significant reduction in the fat layer during ultrasound images after a single therapy of cryolipolysis. In the study by Stevens and Bachelor (2015) [39] who studied 40 patients as topics, ultrasound information specified considerable fat layer lowering.
In a meta-analysis study [40], it wasobserved that reduction of visceral adipose tissue may be by practice exercise without any diet in people with obesity. The study was in agreement with the study by Ismael et al., 2012 [41] who reported in their meta-analysis that practicing aerobic exercise has significant results at decreasing visceral adiposity tissue (VAT).
Katch et al., 2013[42] tested the fat cell volume of fat tissue after the biopsy to research the influence of exercise on subcutaneous adipose tissue. After examining 19 young Caucasian men to exercise for four weeks, the investigators explained that an advanced straighten up practice exercise program may be due to a considerable lowering in adipose cell volume of the abdominal, gluteal, and subscapular areas. While there was no discrimination utilize of applied under the skin fat over the abdominal area, four weeks of the abdominal practice exercise was enough may be due to lowering the fat cell volume.
The results of Kostek et al., 2007 [43] agreed with the result of this study as they found a significant reduction in the subcutaneous fat in the trained arm compared to the untrained arm after twelve weeks of supervised resistance training when measured by the skinfold technique.
Katja et al., 2009 [44] observed considerably reduced fat pad mass and adipocyte volume in the study group than the sedentary controls. Exercise training also encouraged a significant decrease in the number of cells in the visceral fat of great-fat diet-fed rats. Generally, practical exercise has stopped the influences of the diet with high fat on properties of adipose tissue and these outcomes were noticeable in visceral than in under the skin fat.
Pontiroli et al., 2009 [45]found that changes of waist circumference and BMI are the leading forces for changes of both subcutaneous adiposity tissue (SAT) and visceral adiposity tissue (VAT) and that changes of SAT and VAT are correlated to each other. In addition, changes in weight and VAT, are associated with metabolic changes more than changes in SAT, in particular reduction of insulin levels.
There are few studies examining the effect of abdominal exercise on the amount of abdominal fat and reporting conflicting results. Vispute et al., 2011 [46] showed that abdominal exercises were influential to excess abdominal strength but were not influential in lowering the amount of abdominal fat. Many people try to decrease their waistline by just implementing abdominal exercises perhaps may be due to demands made by different abdominal apparatus advertisements. The results of this research can help people to comprehend that abdominal exercise alone is not enough to reduce waistline or under-skin abdominal fat. It is probably essential to contain aerobic exercise only with lowering power intake to have addition appropriate alterations in body fat percentage.
Similar research by Ramírez-Campillo et al., 2013 [47] found that 27 days of abdominal exercise did not promote centralize fat mobilization from the abdominal region.
Conclusion:
It can be concluded that cryolipolysis and abdominal exercises can reduce the abdominal subcutaneous fat, while the combination of both methods in the same program has more significant effects on the abdominal subcutaneous fat in women with central obesity, which may decrease its complications and morbidities.
References
- Navaneelan T, Janz T. Adjusting the scales: Obesity in the Canadian population after correcting for respondent bias. Statistics Canada; 2014.
- Yuniarto A, Sukandar EY, Fidrianny I, Setiawan F, Ketut I. Antiobesity, Antidiabetic and Antioxidant Activities of Senna (Senna alexandrina Mill.) and Pomegranate (Punica granatum L.) Leaves Extracts and Its Fractions. International Journal of Pharmaceutical and Phytopharmacological Research (eIJPPR). 2018 Jun 1;8(3):18-24.
- Mathieu P, Lemieux I, Després JP. Obesity, inflammation, and cardiovascular risk. Clinical Pharmacology &Therapeutics. 2010 Apr;87(4):407-16.
- Blouin C, Jen Y, Lamontagne P, Martel S. The economic impact of obesity and overweight. Institut national de sante publiqué du Québec; 201
- Taltia A, Roy A. Orlistat - an anti-obesity drug - An overview. J Adv Pharm Edu Res. 2017;7(3):190-3.
- GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. New England Journal of Medicine. 2017 Jul 6;377(1):13-27.
- Adeniyi OV, Longo-Mbenza B, Ter Goon D. Female sex, poverty and globalization as determinants of obesity among rural South African type 2 diabetics: a cross-sectional study. BMC public health. 2015 Dec;15(1):298.
- Yassine HN, Marchetti CM, Krishnan RK, Vrobel TR, Gonzalez F, Kirwan JP. Effects of exercise and caloric restriction on insulin resistance and cardiometabolic risk factors in older obese adults—a randomized clinical trial. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2009 Jan 1;64(1):90-5.
- Salama Mohamed KM, El-Tohamy AM, El-Hadidy L. Impact of Virtual Reality on Body Composition in Children With Obesity. International Journal of Pharmaceutical and Phytopharmacological Research. 2017;7(4):26-33.
- Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality. Circulation. 2008 Apr 1;117(13):1658-67.
- Cameron AJ, Zimmet PZ. Expanding evidence for the multiple dangers of epidemic abdominal obesity. Circulation; 117(13):1624–1626.
- World Health Organization. Obesity: preventing and managing the global epidemic. World Health Organization; 2000, page 6 and 9.
- National Institutes of Health (2012): Overweight and obesity statistics.
- Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012 Mar 6;125(9):1157-70.
- Apovian CM, Aronne LJ, Bessesen DH, McDonnell ME, Murad MH, Pagotto U, Ryan DH, Still CD. Pharmacological management of obesity: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism. 2015 Feb 1;100(2):342-62.
- Coleman SR, Sachdeva K, Egbert BM, Preciado J, Allison J. Clinical efficacy of noninvasive cryolipolysis and its effects on peripheral nerves. Aesthetic plastic surgery. 2009 Jul 1;33(4):482-8.
- You T, Murphy KM, Lyles MF, Demons JL, Lenchik L, Nicklas BJ. Addition of aerobic exercise to dietary weight loss preferentially reduces abdominal adipocyte size. International journal of obesity. 2006 Aug;30(8):1211.
- Thomas M, Menon H, D'Silva J. Surgical complications of lipoplasty–management and preventive strategies. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2010 Aug 1;63(8):1338-43.
- Fischer JP, Wes AM, Serletti JM, Kovach SJ. Complications in body contouring procedures: An analysis of 1797 patients from the 2005 to 2010 American College of Surgeons National Surgical Quality Improvement Program databases. Plastic and reconstructive surgery. 2013 Dec 1;132(6):1411-20.
- Jae M, Luscher T, Cosentio F. Obesity. The Lancet. 2008 ;306(9492):119- 127.
- Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AE. Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death–. The American journal of clinical nutrition. 2006 Aug 1;84(2):449-60.
- Richardson CA, Hodges P, Hides JA. Therapeutic exercise for lumbopelvic stabilization: a motor control approach for the treatment and prevention of low back pain. 2004:1-271.
- Mota P, Pascoal AG, Sancho F, Bø K. Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. journal of orthopaedic & sports physical therapy. 2012 Nov;42(11):940-6.
- Vispute SS, Smith JD, LeCheminant JD, Hurley KS. The effect of abdominal exercise on abdominal fat. The Journal of Strength & Conditioning Research. 2011 Sep 1;25(9):2559-64.
- Juan-Recio C, Lopez-Vivancos A, Moya M, Sarabia JM, Vera-Garcia FJ. Short-term effect of crunch exercise frequency on abdominal muscle endurance. The Journal of sports medicine and physical fitness. 2015 Apr;55(4):280-9.
- Misra P, Upadhyay RP, Krishnan A, Vikram NK, Sinha S. A community-based study of metabolic syndrome and its components among women of rural community in Ballabgarh, Haryana. Metabolic syndrome and related disorders. 2011 Dec 1;9(6):461-7.
- ElKafrawi NA, Shoaib AA, Elghanam MH. Measurement of waist circumference as a screening tool for type 2 diabetes mellitus in female patients. Menoufia Medical Journal. 2017 Jan 1;30(1):168–173.
- Ingargiola MJ, Motakef S, Chung MT, Vasconez HC, Sasaki GH. Cryolipolysis for fat reduction and body contouring: safety and efficacy of current treatment paradigms. Plastic and reconstructive surgery. 2015 Jun;135(6):1581–90.
- Krueger N, Mai SV, Luebberding S, Sadick NS. Cryolipolysis for noninvasive body contouring: clinical efficacy and patient satisfaction. Clinical, cosmetic and investigational dermatology. 2014;7:201.
- Ferraro GA, De Francesco F, Cataldo C, Rossano F, Nicoletti G, D’Andrea F. Synergistic effects of cryolipolysis and shock waves for noninvasive body contouring. Aesthetic plastic surgery. 2012 Jun 1;36(3):666-79.
- Nelson AA, Wasserman D, Avram MM. Cryolipolysis for reduction of excess adipose tissue. , 28, 4. 2009 Dec 1;28(4):244-9.
- Klein KB, Zelickson B, Riopelle JG, Okamoto E, Bachelor EP, Harry RS, Preciado JA. Non‐invasive cryolipolysis™ for subcutaneous fat reduction does not affect serum lipid levels or liver function tests. Lasers in Surgery and Medicine: The Official Journal of the American Society for Laser Medicine and Surgery. 2009 Dec;41(10):785-90.
- Zelickson B, Egbert BM, Preciado J, Allison J, Springer K, Rhoades RW, Manstein D. Cryolipolysis for noninvasive fat cell destruction: initial results from a pig model. Dermatologic Surgery. 2009 Oct;35(10):1462-70.
- Zelickson BD, Burns AJ, Kilmer SL. Cryolipolysis for safe and effective inner thigh fat reduction. Lasers in surgery and medicine. 2015 Feb;47(2):120-7.
- Pinto H, Arredondo E, Ricart-Jané D. Evaluation of adipocytic changes after a simil-lipocryolysis stimulus. Cryoletters. 2013 Jan 1;34(1):100-5.
- Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowski D, Anderson RR. Selective cryolysis: A novel method of non‐invasive fat removal. Lasers in Surgery and Medicine: The Official Journal of the American Society for Laser Medicine and Surgery. 2008 Nov;40(9):595-604.
- Dover J, Burns J, Coleman S, Fitzpatrick R, Garden J, Goldberg D, Geronemus R, Kilmer S, Mayoral F, Weiss R, Zelickson B. A Prospective Clinical Study of Noninvasive Cryolipolysis for Subcutaneous Fat Layer Reduction—Interim Report of Available Subject Data: 129. Lasers in Surgery and Medicine. 2009 Jul 1;41:706.
- Carruthers J, Stevens WG, Carruthers A, Humphrey S. Cryolipolysis and skin tightening. Dermatologic Surgery. 2014 Dec 1;40:S184-9.
- Stevens WG, Bachelor EP. Cryolipolysis conformable-surface applicator for nonsurgical fat reduction in lateral thighs. Aesthetic surgery journal. 2015 Jan 1;35(1):66-71.
- Vissers D, Hens W, Taeymans J, Baeyens JP, Poortmans J, Van Gaal L. The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PloS one. 2013 Feb 8;8(2):e56415.
- Ismail I, Keating SE, Baker MK, Johnson NA. A systematic review and meta‐analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Obesity reviews. 2012 Jan;13(1):68-91.
- Katch FI, Clarkson PM, Kroll W, McBride T, Wilcox A. Effects of sit up exercise training on adipose cell size and adiposity. Research Quarterly for Exercise and Sport. 1984 Sep 1;55(3):242-7.
- Kostek MA, Pescatello LS, Seip RL, Angelopoulos TJ, Clarkson PM, Gordon PM, Moyna NM, Visich PS, Zoeller RF, Thompson PD, Hoffman EP. Subcutaneous fat alterations resulting from an upper-body resistance training program. Medicine & Science in Sports & Exercise. 2007 Jul 1;39(7):1177-85.
- Gollisch KS, Brandauer J, Jessen N, Toyoda T, Nayer A, Hirshman MF, Goodyear LJ. Effects of exercise training on subcutaneous and visceral adipose tissue in normal-and high-fat diet-fed rats. American Journal of
Physiology-Endocrinology and Metabolism. 2009 Aug;297(2):E495-504. - Pontiroli AE, Frigè F, Paganelli M, Folli F. In morbid obesity, metabolic abnormalities and adhesion molecules correlate with visceral fat, not with subcutaneous fat: effect of weight loss through surgery. Obesity surgery. 2009 Jun 1;19(6):745-50.
- Vispute SS, Smith JD, LeCheminant JD, Hurley KS. The effect of abdominal exercise on abdominal fat. The Journal of Strength & Conditioning Research. 2011 Sep 1;25(9):2559-64.
- Ramírez-Campillo R, Andrade DC, Campos-Jara C, Henríquez-Olguín C, Alvarez-Lepín C, Izquierdo M. Regional fat changes induced by localized muscle endurance resistance training. The Journal of Strength &Conditioning Research. 2013 Aug 1;27(8):2219-24.
Contact SPER Publications
SPER Publications and
Solutions Pvt. Ltd.
HD - 236,
Near The Shri Ram Millenium School,
Sector 135,
Noida-Greater Noida Expressway,
Noida-201301 [Delhi-NCR] India
