The effect of revascularization of the internal Carotid artery on the Microcirculation of the eye
D.G. Iosseliani*, N.S. Bosha, T.S. Sandodze, A.V. Azarov, S.P. Semitko
Federal State Autonomous Educational Institution of Higher Education I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation, Research and Practical Center of Interventional Cardioangiology, Moscow, Russia.
ABSTRACT
This research studied the changes in the perfusion of the retina and the optic nerve head in patients after carotid endarterectomy and carotid stenting with the use of optical coherence tomography angiography. The study involved 30 patients with hemodynamically significant stenosis (≥ 75 %) of the right or left internal carotid artery (ICA). The patients were divided into two groups: Group 1 — patients after stenting of the ICA (17 patients), and Group 2 — patients after carotid endarterectomy performed from the carotid artery (13 patients). OCT-A performed before the revascularization procedures had not revealed any significant differences in terms of the blood flow density on the side of the stenosed and non-stenosed carotid arteries. In the early postsurgery period, the blood flow density increased in the macular area both at the level of the surface and the deep layer (p < 0.05). It should be noted that the increase in the blood flow density was more pronounced in the area of the capillary plexus and the capillary choroid of the ONH (p < 0.01). The studied parameters obtained after stenting and carotid endarterectomy were not veraciously different. At the follow-up examination, three months after the revascularization procedures, optical coherence tomography angiography showed a moderate decrease in some flow density parameters, compared to the results obtained immediately after the procedure; however, they remained higher than the initial values, both on the affected and the contralateral sides. The first experiment in studying the brain structure microcirculation (the retina and the ONH) after carotid stenting (CS) and carotid endarterectomy (CEAE) showed that after revascularization, the eye retina perfusion parameters increase, which may serve as an indirect confirmation of an improvement in the cerebral perfusion after revascularization of the carotid arteries. The foregoing applies to both the CS and CEAE procedures. However, further accumulation of experience in this area is required for making conclusions.
Keywords: optical coherence tomography (OCT), carotid stenting, carotid endarterectomy, eye retina, revascularization, eye microcirculation
Introduction
Surgical and X-ray endovascular revascularization has taken the leading positions in the treatment of the ischemic state of various organs and tissues. Revascularization of the heart, the brain, the kidneys, the abdominal organs, the extremities, etc. has saved the lives of and returned to normal work many millions of people in the world. Today, there is no doubt that these procedures improve the clinical state of the patients, as well as the blood circulation in the arterial vessels after revascularization. The issues concerning the effect of reperfusion on the state of microcirculation in these organs have been studied to a much lesser extent. An example is the internal carotid artery (ICA) revascularization procedure. It is known that this vessel is responsible for the vascularization of a significant part of the brain, and the impaired blood flow in it may lead to significant and sometimes irreversible dysfunctions of the central nervous system. For example, stenosis of the carotid artery, and, thereby, impaired vascularization of the brain structures are among the most important risk factors for the development of ischemic strokes and transient ischemic attacks. It should be noted that about 15 – 25 % of the diseases of the nervous system are caused by impaired cerebral circulation. In economically developed countries, cerebral stroke ranks third among the mortality causes. It is known that about two-thirds of all ischemic stroke cases are caused by the steno-occlusive lesions of the carotid arteries. For instance, with a stenotic lesion of the ICA by more than 75 %, the likelihood of developing an ischemic stroke during the first year after the diagnosis ranges between 2 and 5 %, and in the presence of clinical manifestations in the form of transient ischemic attacks, the likelihood increases to about 40 %. It should be especially noted that the degree of stenosis of the carotid artery is a fairly clear indicator of the likelihood of a cerebral stroke in the patients, and serves as an objective indication for medical procedures on the vessel [1-3].
Until the end of the eighties of the past century, drug therapy had been mainly used for the treatment of the patients with stenotic lesions of the carotid arteries, while surgical treatment, namely, carotid endarterectomy (CEAE) had been used much less frequently. However, with the introduction of endovascular revascularization of the vessels into the clinical practice, this method has been successfully and widely used for the treatment of stenotic lesions of the carotid arteries. Today, one can confidently say that the main methods of treatment for the patients with clinical manifestations of cerebral vascular insufficiency and carotid stenosis are carotid artery stenting and carotid endarterectomy. In recent years, a sufficient number of randomized studies comparing the two methods in the treatment of the brachiocephalic vessels have been published. These studies have not revealed any significant differences in the immediate and long-term results of treatment with the use of these methods of brain revascularization [4]. Therefore, in such cases, preference should be given to the less traumatic method of treatment, which is stenting of the carotid artery.
In using either method of revascularization of the brain, the degree of impaired blood circulation correction efficiency both at the level of macrocirculation, i.e., the great vessels, and at the level of microvasculature remains the main issue. While concerning large vessels, the results of the treatment may be quite adequately assessed by computed tomography, magnetic resonance imaging, and ultrasound imaging, studying the microvasculature of the brain structures seems to be more complicated [5]. It should be noted, however, that in recent years, the methods that allow a fairly complete study of the blood circulation at the level of microcirculation have appeared. An example is a method of optical coherence tomography (OCT) which may be successfully used for studying the microcirculation of the ocular fundus, which is a structure of the brain, and at the same time, is sensitive not only to the circulatory disorders in the ICA system but also to the disruption of the blood supply to the heart [6].
OCT-A is a relatively new technology that allows non-invasive visualization of the vasculature of the retina and the optic nerve head (ONH) by assessing quantitatively and qualitatively the blood flow in these areas. It should be particularly noted that the blood vessels of the fundus are extremely sensitive in general to the pathological processes in the organism, and in particular, in the pathology of the brain, the nervous system, and the heart [7-9]. In particular, this applies to the processes associated with the impaired vascularization of these structures. It is known that steno-occlusive changes in the ICAs are accompanied by the impaired blood supply to the eyes, which in turn may lead to a sudden or progressive decrease in visual acuity. It is, therefore, logical to assume that reverse changes, i.e., improvement of the blood circulation in the ICA system, may be accompanied by positive changes in the microcirculation of the fundus, and the eye in whole [10, 11].
That said, the task was set to study the microcirculation of the retina and the optic nerve trunk before and after restoring the adequate blood flow in the ICA by stenting or CEAE through OCT-A in the patients with a sharp (> 75 %) stenotic lesion of this vessel.
Materials and Methods
The study involved 30 patients with hemodynamically significant stenosis (≥ 75 %) of the right or left ICA. The patients had been divided into two groups: Group 1 — patients after stenting of the ICA (17 patients), and Group 2 — patients after carotid endarterectomy performed from the carotid artery (13 patients). The clinical characteristics of the patients are shown in Table 1.
|
Table 1: The clinical and anamnestic characteristics of the studied patients |
||
|
|
Group 1 (stenting) (n = 17) |
Group 2 (CEAE) (n = 13) |
|
Age (average) |
70.2 ± 8.3 |
70.9 ± 7.5 |
|
Gender: M F |
8 (47.1 %) 9 (52.9 %) |
7 (53.8 %) 6 (46.2 %) |
|
Previously performed coronary artery bypass grafting (CABG) and/or stenting of coronary arteries |
14 (82.4 %) |
9 (69.2 %) |
|
Stenosis of the left ICA |
7 (41.2 %) |
6 (46.2 %) |
|
Stenosis of the right ICA |
10 (58.8 %) |
7 (53.8 %) |
|
Arterial hypertension |
15 (88.2 %) |
12 (92.3 %) |
As one can see from Table 1, multifocal atherosclerosis was observed in the absolute majority of the patients. Some of them had a history of direct myocardial revascularization and/or stenting of the coronary arteries. It should also be noted that 22 (73.3 %) patients had stenotic lesions of the other carotid artery of varying severity, which, however, did not exceed 70 %.
The criterion for involving the patients in the study was the presence of stenosis of the ICA (≥ 75 %). In most cases, the right ICA had been affected. The patients with severe ocular pathology associated with a reduced permeability of the optical media (cataract) or the presence of vitreoretinal diseases, as well as the patients with acute myocardial infarction and those with serious neurological diseases, including cerebral stroke, were not involved in the study.
Stenting of the ICA was performed following the standard technique with the obligatory use of an anti embolic protective device and balloon post-dilation of the stented area.
CEAE was performed under general anesthesia. After the isolation of the common carotid artery and bolus administration of heparin, the common, external, and the ICAs were separately clamped, and bypasses were placed above the vascular compression to maintain perfusion of the intracranial arteries. After that, the atherosclerotic plaque was removed. The duration of ICA clamping during the surgery averaged 28.4 ± 5.9 minutes. The patients were monitored within 24 hours after CEAE.
OCT-A was performed on a CANON tomograph using an A-scan with a capacity of 70,000 scans per second. The study was performed by the same researcher in completely identical conditions. The ONH area was 4.5 x 4.5 mm2, and the macular area was 3.0 x 3.0 mm2. The comparative analysis was performed for the surface capillary layers of the ONH and the macular area, as well as the deep capillary layer of the macula and the choriocapillaris layer of the ONH. The flow density segmentation was determined automatically for each area and subjected to further analysis.
Before OCT-A, the patients had remained at complete rest for five minutes, after which their blood pressure was measured on the left arm in a sitting position, provided that the patient's arm was exactly at the height of the heart. The patients underwent OCT three times in the following sequence: in Group 1, not earlier than one week before stenting and two-three days after the procedure; in Group 2, also not earlier than one week before carotid endarterectomy and five-seven days after it. Three months after the procedure, all patients in both groups underwent the third follow-up OCT-A on an outpatient basis.
Results
The OCT-A performed before revascularization procedures did not reveal any significant differences in terms of the blood flow density on the side of the stenosed and non-stenosed carotid arteries (p < 0.05). The groups were also comparable from the standpoint of baseline indicators (Table 2).
|
Table 2: Blood flow density in the macular area and at the level of the ONH before revascularization (the ipsilateral and the contralateral side) |
||||
|
OCT-A |
Group 1 |
Group 2 |
||
|
Affected side |
Without ICA stenosis |
Affected side |
Without ICA stenosis |
|
|
Central Surface |
46.42 ± 3.21 |
46.82 ± 3.32 |
45.87 ± 3.57 |
46.76 ± 3.77 |
|
Central Deep |
48.52 + 4.41 |
49.51 ± 4.13 |
47.14 + 4.32 |
49.75 + 3.24 |
|
Surface ONH |
50.31 ± 3.76 |
50.55 ± 3.69 |
49.1 ± 3.95 |
50.12 ± 3.11 |
|
Choroidal ONH |
52.38 ± 4.1 |
53.58 ± 4.57 |
52.13 ± 3.4 |
52.85 ± 3.86 |
In the early postsurgery period, the blood flow density increased in the macular area both at the level of the surface and the deep layer (p < 0.05). It should be noted that the increase in the blood flow density was more pronounced in the area of the capillary plexus and the capillary choroid of the ONH (p < 0.01). The studied parameters obtained after stenting and carotid endarterectomy were not veraciously different (Table 3).
|
Table 3: Blood flow density on the side of the ICA on which the revascularization procedure was performed |
||||
|
OCT-A |
Stenting |
CEAE |
||
|
Before |
After |
Before |
After |
|
|
Central Surface |
46.42 ± 3.21 |
47.79 ± 2.24 |
45.87 ± 3.57 |
46.89 ± 2.91 |
|
Central Deep |
48.52 + 4.41 |
49.96 + 4.11 |
47.14 + 4.32 |
48.69 + 4.05 |
|
Surface ONH |
50.31 ± 3.76 |
51.67 ± 3.12 |
49.1 ± 3.95 |
52.08 ± 3.12 |
|
Choroidal ONH |
52.38 ± 4.1 |
53.95 ± 4.5 |
52.13 ± 3.4 |
54.01 ± 4.02 |
It should be particularly noted that an increase in the flow was also noted on the contralateral side (Table 4).
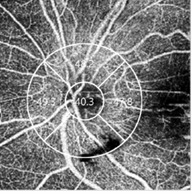
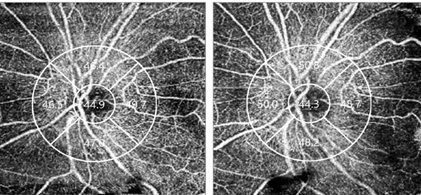
Figure 1 shows the data of OCT-A of the retina in patient O. 58 years old before and at various times after stenting of the right ICA.
|
Table 4: Blood flow density on the contralateral side before and after revascularization |
||||
|
OCT-A |
Group 1 |
Group 2 |
||
|
Before |
After |
Before |
After |
|
|
Central Surface |
46.82 ± 3.32 |
47.03 ± 2.75 |
46.76 ± 3.77 |
47.24 ± 3.84 |
|
Central Deep |
49.51 ± 4.13 |
49.95 ± 3.86 |
49.75 + 3.24 |
50.26 ± 3.56 |
|
Surface ONH |
50.55 ± 3.69 |
51.68 ± 2.95 |
50.12 ± 3.11 |
50.85 ± 3.48 |
|
Choroidal ONH |
53.58 ± 4.57 |
54.13 ± 4.97 |
52.85 ± 3.86 |
53.47 ± 3.73 |
The clinical example of changes in the retinal flow density in 57 years old patient after ICA stenting.
|
|
|
|
|
a — before revascularization |
b — in the next days after revascularization |
c — three months after revascularization |
Figure 1: OCT angiogram of the patient before and after stenting of the right carotid artery. An improvement in the microcirculation three days and three months after the surgery is visible on the slices
At the follow-up examination three months after the revascularization procedures, OCT-A showed a moderate decrease in some flow density parameters, compared to the results obtained immediately after the procedure; however, they remained higher than the initial values, both on the affected (Table 5) and the contralateral side (Table 6).
|
Table 5: Flow density in the macular area and at the level of the ONH immediately after and three months after the revascularization procedure (the ipsilateral side) |
||||
|
OCT-A |
Group 1 |
Group 2 |
||
|
Three days |
Three months |
Three days |
Three months |
|
|
Central Surface |
47.79 ± 2.24 |
47.35 ± 2.27 |
46.89 ± 2.91 |
46.53 ± 3.01 |
|
Central Deep |
49.96 + 4.11 |
50.07 ± 3.52 |
48.69 + 4.05 |
50.12 + 3.12 |
|
Surface ONH |
51.67 ± 3.12 |
51.07 ± 3.21 |
52.08 ± 3.12 |
52.83 ± 3.93 |
|
Choroidal ONH |
53.95 ± 4.5 |
54.01 ± 3.95 |
54.01 ± 4.02 |
54.95 ± 3.17 |
|
Table 6: Flow density in the macular area and at the level of the ONH immediately after and three months after the revascularization procedure (the contralateral side) |
||||
|
OCT-A |
Group 1 |
Group 2 |
||
|
Three days |
Three months |
Three days |
Three months |
|
|
Central Surface |
46.82 ± 3.32 |
47.03 ± 2.75 |
46.76 ± 3.77 |
47.24 ± 3.84 |
|
Central Deep |
49.51 ± 4.13 |
49.95 ± 3.86 |
49.75 + 3.24 |
50.26 ± 3.56 |
|
Surface ONH |
50.55 ± 3.69 |
51.68 ± 2.95 |
50.12 ± 3.11 |
50.85 ± 3.48 |
|
Choroidal ONH |
53.58 ± 4.57 |
54.13 ± 4.97 |
52.85 ± 3.86 |
53.47 ± 3.73 |
Discussion and Conclusion
In 2018, a publication by L. Lahme et al. was published, in which the results of a comparative analysis of OCT data from an angiographic study of the fundus microcirculation in the patients with significant stenosis of the carotid arteries and the carotid arteries not susceptible to stenosing atherosclerosis were presented for the first time. The authors showed that in the patients with hemodynamically significant stenosis of the ICA, there was a significant decrease in the density of the blood flow in the retina and the ONH, compared to similar values in the patients without stenotic lesions of the carotid artery. The same authors showed that in the patients with stenosing lesions of the carotid artery, after CEAE, there was a significant improvement in the blood flow in the retina and the ONH of the eye located in the basin of the carotid artery operated on. Improved blood flow was observed both in the early and late postsurgery periods. This pilot study for the first time showed a stable increase in the blood flow in the retina and the ONH after successful restoration of the blood flow in the stenotic carotid artery through the surgical endarterectomy of an atherosclerotic plaque [12]. Later, two papers were published, in which the authors studied the dynamics of retinal microcirculation through OCT-A in the patients after ICA stenting [12, 13]. Meanwhile, there are no studies based on a comparative analysis of ocular microcirculation through OCT-A in the patients after stenting of the ICA and CEAE. Thus, the authors assume that this research study has been the first in this area.
The study carried out by the authors has shown that after stenting of the carotid artery affected by stenosing atherosclerosis, as well as after CEAE, there has been an improvement in the vascularization of the retina and the ONH not only of the eye located in the basin of the stented carotid artery but also of the other eye. This is probably because, in the absolute majority of the studied patients, the second carotid artery was also affected to a greater or lesser degree. Therefore, restoration of the blood flow in one of the carotid arteries could lead to an improvement in the microcirculation of the other eye as well, perhaps due to the blood circulation in the eye.
Thus, the study performed with a small group of patients has convincingly shown that revascularization of the carotid artery by stenting and CEAE significantly increases the density of the blood flow in the area of the ONH capillary network, of the parapapillary choroid, and, to a lesser extent, in the macular area. From the standpoint of the degree and the nature of the changes in the microcirculation of the eye, there is no significant difference between the methods of carotid artery revascularization (stenting or CEAE). Therefore, it can be argued with a high degree of probability that stenting of the carotid arteries and carotid endarterectomy improves the blood circulation not only in the great vessels but also at the level of microcirculation.
It should also be noted that the first studies of the dynamic changes in the eyes microcirculation after carotid revascularization through OCT-A have shown that this method is effective for determining the state of the microvasculature of the brain structures, in particular, and for comparative assessment of the dynamic changes in the blood supply after various therapeutic procedures. However, it should be remembered that the study of the fundus blood flow through OCT-A is limited in the case of various associated eye diseases.
Finally, for concluding the effectiveness and reliability of the OCT-A method in studying the microcirculation of brain structures, further accumulation of experience and prolonged duration of long-term observation are required.
References
- Jamal AA, Al-Furaih IM, Binsufayan SA, Jamalaldeen MR, Abunohaiah IS, Alhuzaymi AM, Alduhaim AA, Alfaris E. Factors Determining the Choice of Medical Specialty and Work Environment Among Saudi Physicians: Results from A National Cross-Sectional Survey. Int. J. Pharm. Res. Allied Sci. 2018 Apr 1;7(2):58-66
- Shukri AK, Mubarak AS. Factors of Academic Success Among Undergraduate Medical Students in Taif University, Saudi Arabia: A Cross-Sectional Study. Int. J. Pharm. Res. Allied Sci. 2019;8(1):158-170
- Martinez Faller, E., Therese Hernandez, M., Mark Hernandez, A., Risia San Gabriel, J. Emerging Roles of Pharmacists in Global Health: An Exploratory Study on their Knowledge, Perception, and Competency. Arch. Pharm. Pract. 2020;11(1):40-6.
- Brott TG, Howard G, Roubin GS, Meschia JF, Mackey A, Brooks W, Moore WS, Hill MD, Mantese VA, Clark WM, Timaran CH, Heck D, Leimgruber PP, Sheffet AJ, Howard VJ, Chaturvedi S, Lal BK, Voeks JH, Hobson RW 2nd. CREST Investigators. Long-term results of stenting versus endarterectomy for carotid artery stenosis. N Engl J Med. 2016; 374(11): 1021-1031. DOI:10.1056/NEJMoa1505215
- Matsubara S, Moroi J, Suzuki A, Sasaki M, Nagata K, Kanno I, Miura S. Analysis of Cerebral perfusion and metabolism assessed with position emission tomography before and after carotid artery stenting. Clinical article. J Neurosurg. 2009; 111(1): 28-36. DOI: 10.3171/2008.09.17663
- Wang J, Jiang J, Qian YW, Zhang JF, Wang ZL. Retinal and choroidal vascular changes in coronary heart disease: an optical coherence tomography angiography study. Biomedical Optics Express. 2019; 10(4): 1532-1544. DOI: 10.1364/BOE.10.001532
- Spaide RF, Curcio CF. Evaluation of Segmentation of the Superficial and Deep Vascular Layers of the Retina by Optical Coherence Tomography Angiography Instruments in Normal Eyas. JAMA Ophthalmol. 2017; 135(3): 259-262. DOI: 10.1001/jamaophthalmol.2016.5327
- Rijbroek A, Boellard R, Vermeulen E, Lammertsma AA, Rauwerda JA. Hemodynamic changes in ipsi-and contralateral cerebral arterial territories after carotid endarterectomy using positron emission tomography. Surg Neurol. 2009; 71: 668-676.
- Lee Ch-W, Cheng H-Ch, Chang F-Ch, Wang A-G. Optical Coherence Tomography Angiography Evaluation of Retinal Microvasculature Before and After Carotid Angioplasty and Stenting. Scientific Reports. 2019; 9: 14755.
- Alattas OA, Hamdi AA, Mudarba FM, Alshehri AM, Al-Yahya MS, Almotairi SA, Saeed RA, Buamer MM, Alsuwailem MS, Alamri IA. Red Eye Diagnosis and Management in Primary Health Care. Archives of Pharmacy Practice. 2019 Jul 1;10(3).
- Bledzhyants GA, Mishvelov AE, Nuzhnaya KV,
Anfinogenova OI, Isakova JA, Melkonyan RS, Hite GY, Suprunchuk VE, Makova AV, Popov AN, Ovechkin VS. The Effectiveness of the Medical Decision-Making Support System. Electronic Clinical Pharmacologist in the Management of Patients Therapeutic Profile. Artificial intelligence. Pharmacophores. 2019 Apr 28;10(2):76-81. - Lahme L, Marchiori E, Panuccio G, Nelis P, Schubert F, Mihailovic N, Torsello G, Eter N, Alnawaiseh M. Changes in retinal flow density measured by optical coherence tomography angiography in patients with carotid artery stenosis after carotid endarterectomy. Scientific Reports. 2018; 8: 17161. DOI: 10.1038/s41598-018-35556-4
- Bayar SA, Ozturker ZK, Pinarci EY, Ercan ZE, Akay HT, Yilmaz G. Structural Analysis of the Retina and Choroid before and after Carotid Artery Surgery. Current Eye Research. 2020; 45(4): 496-503. DOI:10.1080/02713683.2019.1666994.
Contact SPER Publications
SPER Publications and
Solutions Pvt. Ltd.
HD - 236,
Near The Shri Ram Millenium School,
Sector 135,
Noida-Greater Noida Expressway,
Noida-201301 [Delhi-NCR] India