Prevalence of Polycystic Ovary Syndrome, and relationship with obesity/overweight: cross-sectional study in Saudi Arabia
Khlood Aldossary1*, Atheer Alotaibi2, Khlood Alkhaldi2, Rahaf Alharbi2
1 Assistant Professor of Pharmacy Practice, College of Pharmacy, Princess Nourah Bint Abdulrahman University, 11671, Riyadh, Saudi Arabia. 2 PharmD candidate, college of Pharmacy, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia.
Correspondence: Khlood Aldossary, Assistant Professor of Pharmacy Practice, College of Pharmacy, Princess Nourah Bint Abdulrahman University, 11671, Riyadh, Saudi Arabia. E-mail: Kmaldossary@ pnu.edu.sa; Kmaldossary @ outlook.com
ABSTRACT
Introduction: Polycystic ovary syndrome (PCOS) is a hormonal disease that affects many women worldwide, with symptoms that include insulin resistance, hair growth, irregular menstrual cycles, and in some cases, infertility. Obesity continues to be quite prominent around the world, and there have been some reports of a relationship between obesity and PCOS, although few studies have explored this in the Arab World. Therefore, the objective of this study was to test the association between PCOS and obesity in a population of university students at a major university in Saudi Arabia. Methods: A population-based cross-sectional study, in which an online questionnaire was sent to 150 female students studying pharmacy at Princess Nourah University in Saudi Arabia in March 2020. 100 students responded to the questionnaire, which included questions on medical information, especially ones related to PCOS symptoms. Results: The prevalence of self-reported PCOS was found to be 16%. 19.4% were overweight and 6.1% were obese, while 28% of obese and overweight had PCOS. This indicates a positive association between obesity and PCOS, but no significant relationship between PCOS and being underweight was found. Conclusion: While there is a relationship between obesity and PCOS, it is unclear whether obesity is a risk factor for PCOS or not. However, there should be intervention programs that tackle this relationship. Future studies should explore this relationship further and focus on whether it is a causal relationship or not.
Keywords: Polycystic ovary syndrome; obesity; overweight; Saudi Arabia
Introduction
Polycystic Ovary Syndrome (PCOS) is a common hormonal condition that affects women of reproductive age. This endocrine disorder has been proven to be genetic through twin studies. [1] It is marked by a resistance to insulin,[2] and is often also associated with hyperandrogenism, in which there is a significant increase in hormones more commonly attributed to males, such as androgens, including testosterone. [3] Other symptoms include hirsutism (excessive hair growth in irregular areas), irregular menstrual cycles, infertility, and polycystic ovarian morphology (PCOM), which is the presence of a significant number of preantral follicles within the patients’ ovaries. [3] Women with PCOS are most likely to present to a physician because of infertility, followed by hirsutism and menstrual irregularities. [4]
PCOS is related to metabolic syndrome and its abnormalities [5]. PCOS has been linked to an increased risk of type-2 diabetes, [6] and studies have shown that they are more likely to develop anxiety, depression, and eating disorders.[7] While this disorder is mostly seen among women of reproductive age, symptoms of it have been seen in prepubescent and post-menopausal women. [3] The worldwide prevalence of PCOS (according to the 2003 Rotterdam criterion) has been reported to be between 4% and 21% [8] and is 16% in the Middle East.[9] Some studies have indicated that Middle Eastern women are more likely to develop PCOS than Caucasian and Asian women, but less likely than Black women.[9]
Studies have shown that it is linked to obesity, [10] with one study concluding that 2/3-4/5 of PCOS patients suffer from obesity as well. [11] While this linkage has been explored in international research and some Arab studies, [12] there remains a need to find a measurable analysis of the relationship between PCOS and obesity/being overweight in Saudi Arabia and the Arab world. The prevalence of obesity and its complication such as coronary heart disease, diabetes, hypertension, and hyperlipidemia is increasing nowadays [13]. Overweight and obesity are widespread in developed and rich countries, while malnutrition and low body weight are found mainly in developing countries [14]. Today, adipose tissue, as an active endocrine system, by producing fatty acids and secreting several types of proteins regulates hormones of absorbing and consuming energy [15]. One Saudi study concluded that the prevalence of PCOS in Madinah is 32.5%, [16] yet more research is still needed throughout the rest of Saudi Arabia. Therefore, the main objective of this research is to measure the prevalence of self-reported PCOS among Saudi women and to examine the link between obesity and PCOS. This condition affects a great proportion of women, and it is necessary to quantify this effect, to be accurately informed and equipped to advise on measures for awareness and treatment.
Methods
An online questionnaire was emailed to 150 randomly selected pharmacy students (n=150) from Princess Nourah University to assess the prevalence of self-reported PCO in March 2020. The questionnaire was developed by the team of experts and included information on certain factors for example self-reported height and weight, information related to PCO, medication, and symptoms related to PCO were also collected. Of the total 150 pharmacy students, 100 returned the questionnaire giving the response rate of 66.6%.
Statistical Analysis
One author surveyed the questionnaires and one entered the data for statistical analysis which were then analyzed using statistical software i.e. SPSS version 25.0. Descriptive statistics (frequencies, percentages) were used to describe the categorical study variables. Chi-square was used to see the difference in outcome concerning BMI. BMI was calculated by using weight and height and the following categories were used to categorize the BMI. If your BMI is less than 18.5, it falls within the underweight range. If your BMI is 18.5 to <25, it falls within the normal. If your BMI is 25.0 to <30, it falls within the overweight range. If your BMI is 30.0 or higher, it falls within the obese range.
Results
Data on self-reported PCO was collected from 100 Saudi national pharmacy students. Of the total 100 students, 99% have heard about PCOS. Of total 74 (74%) were of age 21-25 and 16% reported having confirmed diagnosis of PCO and only 6(6%) were taking some medication. Of total 74 students reported about the clinical visit for PCO and among those 31(31%) reported that they have visited the clinic for PCO. Majority 55 (57%) have heard about PCOS from family or friends while 30% have heard from the health care provider. (Fig 1)
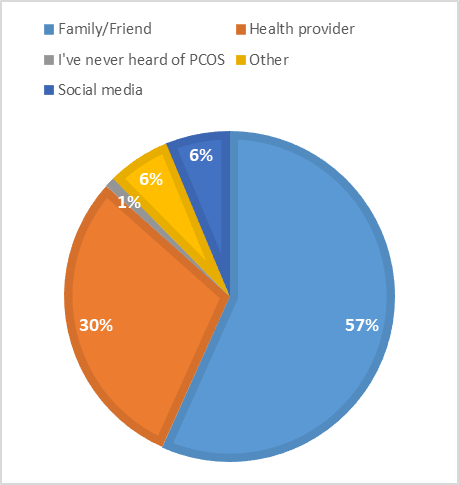
Figure 1: Source of information about PCO among study participants (n=100)
*Others include self-diagnosis, online research
The majority of students reported irregular periods (23%) and hair loss (22%) as the main and only symptoms while other patients reported multiple symptoms and 24(24%) reported no symptoms. (Fig 2)
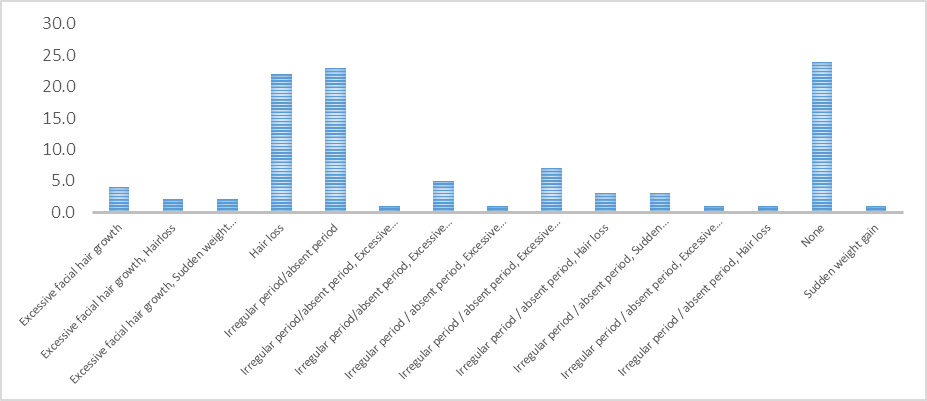
Figure 2: Bar graph showing symptoms of PCOS among study participants (n=100)
BMI was calculated for all the students and we found 57.1% of students fall into normal BMI (18.5 to <25), 19.4% were overweight 25.0 to <30, 6.1% were obese while 17.3% were underweight. Concerning normal weight, 28% of obese/overweight students had PCOS showing positive association of PCOS with obesity/overweight (p-value 0.05) and only 11.8% underweight students had PCOS and the association of PCOS with underweight was not significant with p-value (>0.99). (Table 1)
|
Table 1: Difference in diagnosed and undiagnosed PCOS group concerning BMI among study participants (n=100) |
|||
|
Variables |
Diagnosed PCOS n(%) |
Undiagnosed PCOS n(%) |
P-value |
|
Normal Weight |
6(10.7) |
50(89.3) |
Ref |
|
Underweight |
2(11.8) |
15(88.2) |
>0.99* |
|
Overweight/Obese |
7(28.0) |
18(84.7) |
0.050** |
*p-value for fisher exact
**p-value for chi-square
Discussion
Out of 100 participants, 16 had PCOS, making the prevalence 16%. Moreover, 28% of obese/overweight students had PCOS indicating a significant relationship between obesity and PCOS. The most common symptoms were irregular periods and hair loss, with some reporting multiple symptoms simultaneously, or no symptoms.
Several methodological issues need to be discussed. The study has several limitations. For instance, the sample size was quite small. Students from only one university were included, although it was a major university in Saudi Arabia. All the students also studied in the same department¾pharmacy¾which could have affected their awareness of PCOS and other medical issues. Additionally, they were not asked about other medical issues they may have had or their lifestyles (such as their eating habits or how often they exercise), which could have affected their weight regardless of PCOS. Moreover, some studies have indicated that BMI is not an entirely accurate measure of obesity. [17] Another limitation is that this study only measured the self-report of PCOS without checking the participants’ medical records, which may result in inaccuracies or inconsistencies. However, the study does have several strengths as well. Firstly, the study was conducted on a random sample of students and is a major public educational institution in Saudi Arabia, which is Princess Nourah University.
Our study found that the prevalence of self-reported PCOS is 16%. This coincides with the study conducted by Ding et al., which found that the prevalence of PCOS was 16% among Middle Eastern women. [9] Our findings also fall in line with a study conducted in the USA that found that the worldwide prevalence of PCOS is between 4% and 21%. [8] However, this prevalence was lower than the 35% prevalence which was observed in a study conducted in Madinah, [16] but this could be a consequence of not collecting medical records and instead relying on the students’ self-reporting. Furthermore, this study found that there was indeed a positive association of PCOS with obesity/overweight, while there was no significant relationship between PCOS and being underweight. This is following other studies in the US that show a positive relationship between obesity and PCOS. [18]
The findings of the current study have several implications. For instance, the study found a significant relationship between obesity and PCOS. It is not clear whether obesity is a risk factor or symptom of PCOS, or neither. However, although it is not clear if the relationship is causal or not, obesity should be targeted as a public health issue. Intervention programs should be implemented that target obesity to help women who struggle with PCOS. Doctors should test or check for the symptoms of PCOS among female patients, especially ones that are overweight or obese, to allow for early detection and proper treatment of this disease.
Conclusion
This study found that the prevalence of PCOS among females in a population of Saudi Arabia is 16%. It was observed that there was a significant relationship between obesity and PCOS, while there was no significant association between PCOS and being underweight. Future studies should be longitudinal to explore whether this relationship is causal or non-causal.
Acknowledgment:
The authors would like to acknowledge all pharmacy students at Princess Nourah Bint Abdulrahman University, who participated in this study for their kind support.
This research was funded by the Deanship of Scientific Research at Princess Nourah bint Abdulrahman University through the Fast-track Research Funding Program.
References
- Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI. Heritability of polycystic ovary syndrome in a Dutch twin-family study. The Journal of Clinical Endocrinology & Metabolism. 2006;91(6):2100-4.
- McEwen B, Hartmann G. Insulin resistance' and polycystic ovary syndrome (PCOS)': Part 1. The impact of insulin resistance. Journal of the Australian Traditional-Medicine Society. 2018;24(4):214.
- Azziz R, Carmina E, Chen Z, Dunaif A, Laven JSE, Legro RS, et al. Polycystic ovary syndrome. Nature reviews Disease primers. 2016;2(1):1-18.
- Ovesen PG, Møller N, Greisen S, Ingerslev HJ. Polycystic ovary syndrome I. Clinical presentation and treatment. Ugeskrift for Laeger. 1998;160(3):260-
- Osman NN, Alsahfi SA, Alshubaily F. Effectiveness of Aqueous Extract of Fenugreek Seeds and Flaxseed on Polycystic Ovarian Syndrome in Female Rats. Int. J. Pharm. Res. Allied Sci. 2019;8(4):42-54.
- Gambineri A, Patton L, Altieri P, Pagotto U, Pizzi C, Manzoli L, et al. Polycystic ovary syndrome is a risk factor for type 2 diabetes: results from a long-term prospective study. Diabetes. 2012;61(9):2369-74.
- Månsson M, Holte J, Landin-Wilhelmsen K, Dahlgren E, Johansson A, Landén M. Women with polycystic ovary syndrome are often depressed or anxious—a case-control study. Psychoneuroendocrinology. 2008;33(8):1132-8.
- Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertility and sterility. 2016;106(1):6-15.
- Ding T, Hardiman PJ, Petersen I, Wang F-F, Qu F, Baio G. The prevalence of polycystic ovary syndrome in reproductive-aged women of different ethnicity: a systematic review and meta-analysis. Oncotarget. 2017;8(56):96351.
- Goudas VT, Dumesic DA. Polycystic ovary syndrome. Endocrinology and metabolism clinics of North America. 1997;26(4):893-912.
- Zhang J, Hu J, Zhang C, Jiao Y, Kong X, Wang W. Analyses of risk factors for polycystic ovary syndrome complicated with non-alcoholic fatty liver disease. Experimental and therapeutic medicine. 2018;15(5):4259-64.
- Shousha WG, Zaki ME, El Bassyouni HT, Abdo SM, Mohamed SM. Risk factors in obese Egyptian women with polycystic ovary syndrome. Middle East Journal of Medical Genetics. 2018;7(1):7.
- Ni Gusti Made Ayu Dwi Adhi Suastuti, Ni Wayan Bogoriani, Anak Agung Bawa Putra. Activity of Hylocereus Costarioensis’s Extract as Antiobesity and Hypolipidemic of Obese Rats. Int. J. Pharm. Res. Allied Sci. 2018;7(1):201-208
- Mahassni SH, Munshi MA. Ground Lepidium Sativum Linn Seeds Mixed with The Regular Diet of Rats Lead to Higher Body Weight and Body Weight Gain. Pharmacophores. 2019;10(4):49-56.
- Ashtiani AR, Vahidian-Rezazadeh M, Jafari M, Galdavi R, Mohammad M. Study of Changes in The Plasma Levels of Chemerin of Women with Overweight and Obese During a Period of Endurance Training On a Cycle-Ergometer Using Hydroalcoholic Extract of Urtica. Pharmacophores. 2018;9(2):72-9.
- Alraddadi SM, Borzangi KA, Almuher EM, Albaik AF,
Aljawad LA, Shaqroon AA, et al. Prevalence of polycystic ovarian syndrome with associated risk factors and impact on well-being among women in reproductive-aged (18-45) years in Al-Madinah 2017. World Journal of Pharmaceutical Research. 2018;7(4):231–47. - Rothman KJ. BMI-related errors in the measurement of obesity. International journal of obesity. 2008;32(3): S56-S9.
- Legro RS, editor Obesity, and PCOS: implications for diagnosis and treatment, 2012: Thieme Medical Publishers.
Contact SPER Publications
SPER Publications and
Solutions Pvt. Ltd.
HD - 236,
Near The Shri Ram Millenium School,
Sector 135,
Noida-Greater Noida Expressway,
Noida-201301 [Delhi-NCR] India
