Family support for patients with stroke: a systematic review
Cecep Eli Kosasih 1*, Busakorn Punthmatharith 2, Umaporn Boonyasopun3
1 PhD., Faculty of Nursing, Universitas Padjadjaran, Jl Raya Bandung –Sumedang KM 21, Sumedang, West Java, Indonesia. 2 PhD., Srisavarindhira Thai Red Cross Institute of Nursing, Rama IV Rd, Bangkok Thailand. 3 PhD., Faculty of Nursing, Prince of Songkla University, Hat Yai Campus, Thailand.
ABSTRACT
Background and aims: Roles and family support are crucial in the treatment and rehabilitation of stroke patients. This review aimed to identify the recent intervention, outcome, domain, benefit, and strategies of family support for stroke patients. Methods: A systematic search of PubMed, ProQuest, Science direct, and CINAHL databases using the keywords family support for stroke, intervention, and outcome measures yielded 103 articles. This initial search was subjected to further analysis using the following inclusion criteria: (1) Articles were written in English; (2) Articles were published between 2000-2018; (3) Articles were quantitative study; (4) Articles focused on family support for stroke patients. The exclusion criterion was no duplicated articles. The data collected showed that the interventions were focused on both the stroke patient and their family. Results: Several outcome measurements used to determine the success of family support. The outcome included physical, psychological, social, quality of life, cognitive and economic aspects. The domain included informational, practical, and psychological support. Conclusion: The family support benefitted both the patients and their families. Family support is highly beneficial to accelerate recovery from stroke.
Keywords: Family support of stroke, intervention, outcome measures
Introduction
Stroke is a common problem in the world. The incidence of stroke increases each year not only in developed countries but also in developing countries. Each year in the United States about 795,000 people experience a new or recurrent stroke [1]. Moreover, in developing countries such as in Indonesia, the incidence of stroke is the leading cause of death with over 300 per 100,000 [2]. Stroke patients experience severe problems due to stroke attacking the nervous system. It leaves residual symptoms and treatment of disability which needs a long period for recovery. Healing stroke patients take a long time not only in hospitals but also continues at home with rehabilitation, assisted by their family [3].
Stroke patients experience neurological deficit disorder caused by brain damage due to decreased blood flow to the brain [4, 5]. Most patients who experience disability after stroke are allowed to return home. Family members help patients perform daily activities and sometimes patients are highly dependent on others. Thus, patients need a carer in the rehabilitation process to help while their bodies recover. Roles and family support are crucial in the treatment and rehabilitation of stroke patients. Several studies revealed that family support enhances the recovery of stroke patients [6-8]. The patient receives many benefits from stroke rehabilitation. The role and support of the family are essential to determine the successful rehabilitation of post-stroke patients.
Various articles in the literature review describe social support for stroke. One study reviewed the effects of social support on mood status post-stroke [9]. Another study revealed the support needed from family caregivers to stroke survivors from the hospital to home [10]. Also, a study reviewed supportive care needs among caregivers of individuals following stroke [11]. However, few articles were concerned about; the intervention provided to support the patient and family, the outcomes of family support, the domain of family support, the benefits of family support, and the strategies of family support for the stroke patient. Therefore, it is necessary to explore articles related to intervention, outcomes, domain, benefits, and strategies of family support for stroke patients as evidence of best practice for health workers, especially for nurses.
This article provides a clear understanding of family support, the role of the family and the impact of family support for the successful treatment of stroke patients. Moreover, it provides evidence for the implementation of appropriate nursing care in hospitals and/or community services. This literature review aimed to identify family support intervention, outcomes of the family support, domain of family support, benefits of family support, and strategies of family support.
Material and Methods
This study focused on intervention articles regarding family support. The literature search strategy was carried out as follows. Published literature using PubMed, ProQuest, Science direct, and CINAHL databases were searched. The following terms were used as keywords: family support and stroke, family intervention and stroke, and family participation and stroke. Results from this initial search were subjected to further analysis using the inclusion criteria: (1) Articles were written in English; (2) Articles were published between 2000-2015; (3) Articles were conducted using quantitative methods; (4) Articles focused on family support for stroke patients. The exclusion criteria were no duplicated articles.
The initial search revealed 103 articles. From these data, the search was further refined using keywords. About 89 articles were excluded from the analysis due to not meeting the inclusion criteria or were duplicate articles, leaving only 14 articles. The majority of studies used a randomized control trial (n = 9) and comparative study studies (n = 5). One article used repeated multivariate analysis (see Table 1). The articles were from several countries: United Kingdom (n = 3), Ireland (n = 1), United States (n = 1), Greece (n = 1), Australia (n = 1), Japan (n = 3), Thailand (n = 1), Taiwan (n = 1), India (n=1) and Spain (n=1).
|
Table 1. Summary of family support for stroke patients |
|||||
|
No |
Author |
Methods |
Design |
Outcome measures |
Benefit |
|
|
İnci, F. H. & Temel, A. B. (2016) n = 70 |
This was a randomized controlled trial. The sample consisted of 70 female family caregivers (34 experimental, 36 control group). Data were collected three times (pretest-posttest, follow-up test). |
Randomized control trial |
The Family Index of Regenerativity and Adaptation-General. |
Improvement of the components of the resilience of family caregivers of stroke patients. |
|
|
Malini, (2015) n = 240 |
The study group (experimental group) participants were instructed to enroll in the self-help groups (support group) of their village. Following this, they were taught about the importance of such self-help groups and were asked to participate in the group meetings, held every 15 days. While the study group participants attended a total of six meetings over 3 months. |
True experimental pretest and post-test design
|
The Family System Strength questionnaire. |
Improving the overall well-being of the caregivers of stroke patients |
|
|
Aguirrezabal, A., Duarte, E., Rueda, N., Cervantes, C., Marco, E., &Escalada, F. (2013) n=241 |
After the first week of admission, patients and carers of the intervention group attended to a single educational 2 hour-session. It consisted of an information and carer training class in the neurorehabilitation unit, managed by specially trained members of the multi-disciplinary RHB team (nursing, occupational therapy, and physiotherapy). |
A nonrandomized, controlled trial |
A satisfaction questionnaire described by Pound |
Systematic active information, training and community support provision for stroke patients and carers improves satisfaction with stroke rehabilitation programs and support received after hospital discharge. |
|
|
Hirano, Maeshima, Osawa, Nishio, Takeda, Baba, Kigawa (2012) n = 49 |
The subjects were divided into two groups: a family participation group, in which voluntary training was performed with family members (21 patients), and a non-family participation group, in which voluntary training was performed with a physical therapist (28 patients). The groups were compared by background, cognitive and physical function, post-admission course, and outcome.
|
Comparative study |
The Mini-Mental State Examination, the Japan Stroke Scale [12], and Brunnstrom Recovery Stage and knee extension strength/body weight ratio.The functional independence measure (FIM) |
Voluntary training with family participation was effective in shortening the length of hospital stay and in improving the rate of home discharge in a convalescent rehabilitation ward |
|
|
Oupra, Griffiths, Pryor, and Mott (2010) n = 280 |
A nurse-led Supportive Educative Learning. Program for family caregivers (SELF) comprises didactic education sessions, hands-on training for family caregivers, a booklet for family caregivers describing stroke care and three follow-up phone calls. Caregivers of patients admitted to the intervention hospital following an acute stroke received the intervention, while caregivers of patients admitted to the comparison hospital received the usual care provided at the hospital. |
a non-randomized comparative study with concurrent controls, using a two-group pre-test and post-test design |
The GHQ-28 Thai version, The Caregiver Strain Index [13]. |
Providing education and support to the family caregiver of stroke survivors can reduce caregiver strain and enhance their quality of life |
|
|
Osawa & Maeshima (2010) n =34 |
Family participation. This study compared the improvement at 3 weeks among patients treated with conventional exercise sessions and a program including the participation of family members. |
Comparative study |
The Behavioral Inattention Test (BIT) and a laterality index (LI). The River-mead Mobility Index (RMI), and the Barthel index |
Family participation improved not only the mobility but also USN, suggesting that it can make important contributions to acute stroke rehabilitation |
|
|
Shyu, Kuo, Chen, and Chen (2009) n = 158 |
A caregiver oriented intervention program consisting of hospital health education and occasional discharge referrals and the intervention. The program, consisting of both in-hospital and post-hospital components. A caregiver-oriented intervention program was designed to increase caregiver preparedness, to enhance caregiver perception of balance between competing needs and to satisfy specific needs during the transition between hospitalization and discharge. Longitudinal data were analyzed by the generalized estimating equation approach |
A randomized experimental design |
Short Form (SF-36) Taiwan version, The Family Caregiving Consequence Inventory (FCCI), The Chinese Barthel Index (CBI)
|
Improving the quality of care provided by family caregivers to older patients with stroke and decreasing the likelihood of their institutionalization |
|
|
Gaag, Smith, Davis, Moss, Cornelius, Laing, & Mowles. (2005) n = 38 |
A range of group therapies for people with aphasia and their relatives and counseling for individuals and couples Participants were recruited from the waiting list. They had been offered an induction program by center staff. An induction program consisting of a once-weekly 2-h session spread over seven weeks. This induction consisted of joint and separate therapy groups for the individual with aphasia and their relative/carers. After this, individuals made their own choices about further group therapy.
|
Before and after study |
The EuroQol (EQ-5D), the Stroke and Aphasia Quality of Life Measure (SAQoL-39), the Communication Effectiveness Index (CETI), the caring role measured using the Carer’s Assessment of Difficulties Index (CADI). |
This therapeutic approach has an impact on the quality of life and communication for people with aphasia and their relatives |
|
|
Mant, Winner, Roche, & Wade (2005) n = 212
|
A stroke family support organizer (FSO) provides information, emotional support, and liaison with other services. Patients admitted to hospital with acute stroke who had a close carer were assigned to receive family support or normal care. Families were visited at home by a researcher 12 months after the stroke, and a series of questionnaires were administered to the patient and carer.
|
A single-blind randomized controlled trial. Randomized controlled trial |
For carers the Frenchay activities index, GHQ-28, the Dartmouth Coop chart, and five dimensions of the SF-36 For patients: BarthelIndex, RivermeadMobility Index, FrenchayActivities Index, London Handicap Scale, HADS, DartmouthCo-op Chart. The Lower Limb (LL) section of the Fugl-Meyer Assessment (LL-FMA), Motor |
Family support is effective for carers, but different approaches need to be considered to alleviate the psychosocial problems of stroke patients FAME intervention can serve to optimize patient recovery and family |
|
|
Kalra, Evans, Perez, Melbourn, Patel, Knapp, Donaldson. (2004) n = 300 |
Training caregivers in basic nursing and facilitation of personal care techniques. All patients were managed on a stroke rehabilitation unit with established multidisciplinary practice and received conventional care following existing guidelines. In addition to conventional support, caregivers allocated to have training |
A single, blind, randomized controlled trial |
Modified Rankin scale, BarthelIndex and FrenchayActivities Index, Hospital Anxiety and Depression Scale, and EuroQolVisual Analogue Scale and Caregiver Burden Scale |
Training caregivers during patients’ rehabilitation reduced costs and caregiver burden while improving psychosocial outcomes in caregivers and patients at one year |
|
|
Michael S Clark (2003) n = 62 |
The stroke information package and three visits from a social worker trained in family counseling. Data were collected on admission to and discharge from rehabilitation, and again six months later Stroke information package and three visits from a social worker trained in family counseling. |
A two-group randomized controlled trial. |
Family Assessment Device (FAD), Barthel Index (BI), Adelaide Activities Profile (AAP), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), Mastery Scale (MS), SF-36.
|
Maintained family functioning, and in turn led to improved functional and social patient outcomes. |
|
|
Maeshima, Ueyoshi, Osawa, Ishida, Kunimoto, Shimamoto, Matsumoto, Yoshida. (2003) n = 60 |
Patient exercises with the support of family members. Comparison of improvement at 2 wk between conventional exercise sessions and a program also including the participation of family members. |
Comparative study |
An isokinetic machine. the Rivermead Mobility Index |
Family participation is an important contributor to stroke rehabilitation. |
|
|
Grant, Elliott, Weaver, Bartolucci, Giger. (2002) n = 74 |
Social problem-solving telephone partnerships (SPTPs). The intervention consisted of an initial 3-hour home visit between a trained nurse and the family caregiver within 1 week after discharge to begin problem-solving skill training. This initial session was followed by weekly (the first month) and biweekly (the second and third month) telephone contacts. |
A randomized 3-group repeated-measures experimental design |
Short Form Health Survey (SF-36), the sixth-grade version of the Social Problem-Solving Inventory, The Client Satisfaction Questionnaire, the 20-item Center for
|
Problem-solving training may be useful for family caregivers of stroke survivors after discharge from rehabilitative facilities |
|
|
|
|
|
Epidemiological Studies Depression Scale, the Preparedness for Caregiving Scale, the Caregiving Burden Scale, |
|
|
|
Mant, Carter, Wade, & Winner (2000) n = 590 |
The Family-Support Organizer (FSO) All participants in the family-support group received Stroke Association information leaflets and were left a contact number for the FSO Patients with acute stroke admitted to hospitals in Oxford, UK, were assigned family support or normal care within 6 weeks and after 6 months of stroke. |
A single-blind randomized, controlled trial |
For carers, knowledge about stroke FrenchayActivities Index, general health questionnaire-28 scores, Caregiver Strain Index, Dartmouth Coop Charts, short-form 36 (SF-36), and satisfaction scores, and, For patients, knowledge about stroke and use of services, Barthel Index, RivermeadMobility Index, FrenchayActivities Index, London Handicap Scale, Hospital Anxiety and Depression Scales, Dartmouth Co-op Charts, and satisfaction |
Family support significantly increased social activities and improved quality of life for carers, with no significant effects on patients |
|
|
Tsouna-Hadjis, Vemmos, Zakopoulos, Stamatelopoulos (2000) n = 43 |
Family social support Assessment of first-stroke patients’ functional status, depression, and social status before discharge and at 1, 3, and 6 months after stroke onset, in comparison with the amount of family social support, received |
Repeated multivariate analysis |
The Scandinavian Stroke Scale (SSS), the BarthelIndex, the ZungScale, the Social Scale, the Family Social Support (FSS) Scale. |
High levels of family support instrumental and emotional are associated with progressive improvement of functional status, mainly in severely impaired patients, while the. psychosocial status is also affected
|
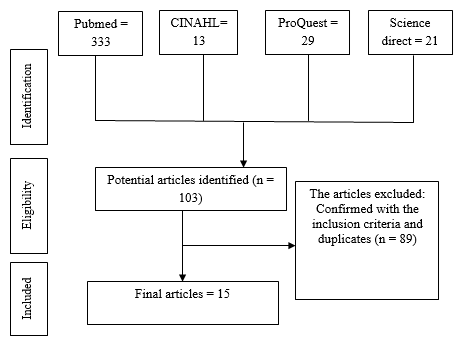
Fig. 1. Article identification and selection process.
Results and Discussion
Results
The results were revealed from the analysis of the selected articles. Regarding the purpose of the study, it was comprised of the intervention of family support, the outcome of the family support, domain of family support, benefits of family support for stroke patients and their family, and strategies of family support for patients with stroke. The articles reviewed were identified based on the purpose of the study. The details of the results were as follows.
- The intervention of Family support
The method of intervention was divided into two classifications; giving support to the family and also patients with stroke and their families. The intervention focused on the training of the family. Besides the intervention of family support focusing on both patients with stroke and their families, it also comprised of providing support for the stroke patient. Eleven articles mentioned providing support for both patients and their families.
The intervention for families of stroke patients was provided by teaching certain techniques by training the families so they were able to provide support to the stroke patient. The training consisted of providing an informational package [14, 15]. A nurse-led Supportive Educative Learning program for family caregivers (SELF) was comprised of didactic education sessions, hands-on training for family caregivers and a booklet for family caregivers [16, 17]. The family conducted voluntary training to participate in caring for stroke patients [7, 8, 18].
The family support organizer also provided support to stroke patients and their families [19, 20]. Another study conducted a range of group therapies for people with aphasia and their relatives as well as counseling for individuals [21]. Also, the intervention involved the family when conducting exercise for stroke patients with the support of family members [22].
- The outcomes of family support
The articles showed that the outcome of the family support comprised of functional status, social recovery, perceived health status, family functioning, depression, anxiety, and mastery, quality of care, quality of life, self-care ability, family caregivers’ strain, knowledge about stroke, social activities and handicap, emotional state, satisfaction with services, activity index, mobility, activity daily living (ADL), general health, social problem-solving abilities, satisfaction with health care, caregiver preparedness, caregiving burden, cognitive and physical function, the carers’ perception, and cost to health and social services. The outcomes included stroke patient and family outcomes.
The stroke patient outcomes consisted of functional status, social recovery, perceived health status, depression, anxiety, and mastery, quality of life, and self-care ability, knowledge about stroke, social activities and handicap, emotional state, satisfaction with services, activity index, mobility, activity daily living (ADL), general health, satisfaction with health care, cognitive and physical function. The family outcomes included family functioning, quality of care, quality of life, family caregivers’ strain, knowledge about stroke, social problem-solving abilities, satisfaction with health care, caregiver preparedness, caregiving burden, the carers’ perception, and cost to health and social services.
The outcomes measured family support using both the stroke patient and their family. The functional status of the stroke patient was measured by Barthel Index (BI), Adelaide Activities Profile (AAP), FrenchayActivities Index, the Lower Limb (LL) section of the Fugl-Meyer Assessment (LL-FMA), Motor Assessment Scale, the Berg Balance Scale, the 6-minute walk test, the Reintegration to Normal Living Index and the Nottingham Extended Activities of Daily Living Index, the Behavioral Inattention Test (BIT) and a Laterality Index (LI), Rivermead Mobility Index, London Handicap Scale, the Functional Independence Measure (FIM), Mastery Scale (MS), and the Communication, Effectiveness Index (CETI),
The psychological state was measured by Hospital Anxiety and Depression Scale (HADS), Geriatric Depression Scale (GDS), the 20-item Center for Epidemiological Studies Depression Scale, the Mini-mental State Examination and the Zung Scale. Quality of life was measured by the EuroQol (EQ-5D), the Stroke and Aphasia Quality of Life Measure (SAQoL-39), Dartmouth Coop Charts, satisfaction scores, and the Client Satisfaction Questionnaire. Health status was measured by short form (SF-36), and general health questionnaire-28 scores. To measure the severity of stroke the Scandinavian Stroke Scale (SSS) was used.
The families as carers also have several measurement outcomes. For the carer, the outcome was measured by Family Assessment Device (FAD), the Family Caregiving Consequence Inventory (FCCI), the Caregiver Strain Index [13], the Social Problem-Solving Inventory, the Preparedness for Caregiving Scale and the Caregiving Burden Scale. The caring role was measured using the Carer’s Assessment of Difficulties Index (CADI), the Social Scale and the Family Social Support (FSS) Scale.
- Domains of family support
Family support for stroke patient and their families have several domains including practical, spiritual, psychological, informational, emotional, and physical [23]. From the articles, it was found that most of the studies provided informational domains to subjects. Almost all the studies provided practical support [6-8, 16, 17, 21, 22, 24]. Few studies provide psychological support [14, 19, 24]. Only half of the studies were conducted at home or by phone.
- Benefits of family support for patients with stroke and their family
There were many benefits of family support for the family. Support can help maintain family functioning, and in turn lead to an improved functional, optimal adjustment to living with stroke [14]. Improved quality of care was provided by family caregivers to older patients with stroke [15], reduced caregiver strain, enhanced their quality of life and increased their social activities [17, 19], reduced costs and caregiver burden, and improved psychosocial outcomes in caregivers [16]. Thus, family support will help family to face problems while caring for stoke patients.
The benefits of family support for stroke patient could improve social outcomes for patients [14, 16], decrease the likelihood of their institutionalization [15], served to optimize patient recovery [6], shorten the length of hospital stay and improve the rate of home discharge in a convalescent rehabilitation ward [7], have an impact on quality of life and communication for people with aphasia and their relatives [21], be an important contributor to stroke rehabilitation [22], and was associated with progressive improvement of functional status and psychosocial status [24]. Another benefit of family support was decreased length of stay, cost, and family satisfaction [25, 26]. Those benefits are useful in stroke recovery both physically and psychosocially.
- Strategies of family support for patients with stroke
There were several strategies of support offered to stroke patients and their families. Those strategies were informational packages, giving booklets, home visits, follow up phone calls, hands-on training, family participation/assistance in exercise, emotional support and counseling. Some of them were mixed. The strategies were conducted both in the hospital and the home setting.
An information package was designed to provide general information (stroke and its consequences, highlight measures to reduce the risk of further stroke, provide practical coping suggestions, and give information about community services and support structures) for stroke patients and their families [14, 16, 20]. Another study provided an individualized discharge health educational consultation [15]. Also, an information program was conducted for the family that comprised of didactic education sessions [17]. To provide comprehensive support for stroke patients giving and information booklet is one effective strategy health provider can use.
Home visits were conducted several weeks after discharge to detect/resolve problems [14, 15, 18]. Another form of home visit used follow-up phone calls [17]. This contact enabled the health provider to discuss problems, provide suggestions for care, and provide support to the caregiver.
The hands-on training was conducted to prepare the family for the care of stroke patients. The training comprised lifting and handling techniques, facilitation of mobility and transfers, continence, assistance with personal activities of daily living and communication, tailored to the needs of individual patients [16, 17]. Problem-solving skill training also was given to the family [18].
The family participated in the exercise of stroke patients. The participation of the family consisted of standup exercises, transfer from chair to chair and gait exercises [8, 22] and had an emphasis on transferring, walking, and stair climbing/descending [7]. Family participation took the form of support from the family member while the stroke patient underwent routine exercise.
Emotional support and counseling were part of family support services [20]. Another study provided counseling for individuals and couples with aphasia [21]. The support given helped stroke patients and their families to solve psychological problems during rehabilitation from stroke.
The analysis revealed a model of family support. The model of family support for patients with stroke can be seen in figure 2. This figure showed that there was a relationship between the components of family support.
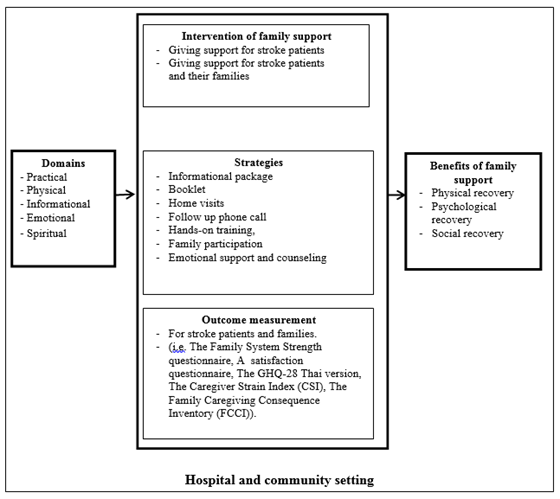
Figure 2. Model of family support for patients with stroke
Discussion
This review has shown the benefits of family support for stroke patients and their families concerning both psychological and physiological outcomes. This is useful for health workers and family caregivers while providing care for stroke patients. Several interventions can be applied to the family of stroke patients with certain outcomes.
The method of intervention in most of the studies reviewed was providing an informational package as the main procedure in family support. It was important as the caregiver needs specific knowledge of procedures and an understanding of certain complications that may develop [27]. Providing information to stroke patients and their families will increase stroke knowledge, as effective stroke knowledge will facilitate a better recovery [14, 28]. This intervention will prepare the family to take care of the stroke patient during acute care and post-discharge. However, the informational package should be given with another form of intervention, since it cannot be an effective intervention by itself.
The outcomes of family support intervention include physical, psychological, social, quality of life, cognitive and economic aspects. Physical outcomes consist of functional status, self-care ability, mastery, activity index, and activity daily living. Barthel Index (BI), Adelaide Activities Profile (AAP) and FrenchayActivities Index are the instruments used to measure the functional status. The Barthel Index was designed to assess the degree of independence in 10 activities of daily living [29]. Measurement of the functional status of stroke patients will determine the ability of a patient to conduct an activity independently.
Psychological outcomes consist of depression, anxiety, emotional state and satisfaction with the services. The psychological state of stroke patients measured by tools such as the Hospital Anxiety and Depression Scale (HADS), Geriatric Depression Scale (GDS), the 20-item Center for Epidemiological Studies Depression Scale, the Mini-mental State Examination, and the ZungScale. The psychological state influences the recovery of stroke. Behavioral and psychological levels were linked as feelings of stress can adversely impact the practice of health behavior [30]. Social outcomes are also essential in the recovery of stroke. The social problem-solving ability of family support can be measured by the Social Problem-solving Inventory for Family Caregiver [18]. The quality of life of stroke patients determines the outcome of family support, it is beneficial to use EuroQol (EQ-5D), and Short Form (SF-36) to assess this. Cognitive outcomes include knowledge about stroke, cognitive function, and the carers’ perception. These outcomes are needed to explore the ability of patients and their families after providing informational support through health workers. The patient and their family need to attain enough knowledge about stroke, thus they can provide appropriate health maintenance in rehabilitation from stroke. Another outcome that plays an important role is a family function such as family caregivers’ strain, caregiver preparedness, caregiving burden, and economic aspects including the cost to health and social services.
According to the results, it was found that most of the articles provided informational and practical support. These forms of support influence the success of family support. However, one form of support for the stroke patient was omitted, spiritual support. The stroke patient needs not only informational and practical support, but also spiritual, psychological, and emotional support [23, 31]. Stroke patients and their families also need comprehensive support from health workers to enhance the recovery process. Spiritual needs were regarded as the need for religious support and carrying out usual rituals within physical limitations during rehabilitation [31].
The benefits of family support are for both the family and stroke patients. Family support helps patients and their families in the process of recovery from stroke. Family support enhances family functioning, optimal adjustment living with stroke, optimizes patient recovery, and progressive improvement of functional status and psychosocial status. Most stroke patients suffer from the impact of stroke. Thus, family support will help the patient and their family reduce morbidity and mortality from stroke.
Conclusion
Health workers can provide family support intervention for stroke patients and their families from the acute care stage in the hospital to the rehabilitation phase at home. The intervention can be through informational package and basic needs training for the family, psychological, social, and spiritual intervention. These interventions will help the family and stroke patients recover from the complications of a stroke. Several outcome measurements can be used to determine the success of family support. The outcomes of family support intervention include physical, psychological, social, quality of life, cognitive and economic aspects. Family support is beneficial for patients and their families. It can increase the quality of life of stroke patients during hospitalization and rehabilitation from stroke.
Implications for Nursing Practice and Research
Family support is a direct action of nursing care by encouraging family members to participate in caring for the stroke patient by providing in hospital and home-based care in the community. Although family support consists of multidisciplinary collaboration, nursing plays an important role in coordinating and applying support for stroke patients and their families. Nurses can expand their professional role in helping patients to accelerate stroke recovery. Since stroke patients need comprehensive support and there are limitations of support intervention, a comprehensive approach that involves all domains of support is needed for application in nursing practice. Further research should be conducted using physical, informational, psychological, social, and spiritual support. The articles reviewed revealed that nurses can use the findings to apply appropriate nursing interventions for stroke patients and their families. For example, the nurses can apply a supportive educative learning program for family caregivers, a caregiver oriented intervention program, train caregivers in basic nursing and facilitation of personal care techniques, and facilitate social problem-solving telephone partnerships. However, spiritual support is rarely applied in the support of stroke patients. This spiritual aspect can influence the health status of the stroke patient.
Conflict of Interest
The authors declare there is no conflict of interest.
Acknowledgement:
We thank the Ministry of Research, Technology and Higher Education of the Republic of Indonesia and Graduate School Prince of Songka University Thailand.
References
- Burton LJ, Tyson S, McGovern A. Staff perceptions of using outcome measures in stroke rehabilitation. Disability and Rehabilitation. 2013 May 1;35(10):828-34. Epub 2012/08/2 doi: 10.3109/09638288.2012.709305. PubMed PMID: 22900574.
- Hoy DG, Rao C, Hoa NP, Suhardi S, Lwin AM. Stroke mortality variations in S outh‐E ast A sia: empirical evidence from the field. International Journal of Stroke. 2013 Oct;8:21-7.
- Hunt R. Community-based nursing: Philosophy or setting?. AJN The American Journal of Nursing. 1998 Oct 1;98(10):44-7.
- Bellou P, Gerogianni KG. The contribution of family in the care of patient in the hospital. Health science journal. 2007 Jul 1(3).
- Hildebrand M, Brewer M, Wolf T. The impact of mild stroke on participation in physical fitness activities. Stroke research and treatment. 2012;2012.
- Galvin R, Cusack T, O'Grady E, Murphy TB, Stokes E. Family-mediated exercise intervention (FAME) evaluation of a novel form of exercise delivery after stroke. Stroke. 2011 Mar;42(3):681-
- Hirano Y, Maeshima S, Osawa A, Nishio D, Takeda K, Baba M, Kigawa H. The effect of voluntary training with family participation on early home discharge in patients with severe stroke at a convalescent rehabilitation ward. European neurology. 2012;68(4):221-8.
- Osawa A, Maeshima S. Family participation can improve unilateral spatial neglect in patients with acute right hemispheric stroke. European neurology. 2010;63(3):170-5.
- Salter K, Foley N, Teasell R. Social support interventions and mood status post stroke: a review. International journal of nursing studies. 2010 May 1;47(5):616-25.
- Cameron JI, Gignac MA. “Timing It Right”: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient education and counseling. 2008 Mar 1;70(3):305-14.
- MacIsaac L, Harrison MB, Godfrey C. Supportive care needs of caregivers of individuals following stroke: a synopsis of research. Can J Neurosci Nurs. 2010;32(1):39-46.
- Goossens S, Radaelli E, Blanchet O, Durinck K, Van der Meulen J, Peirs S, Taghon T, Tremblay CS, Costa M, Ghahremani MF, De Medts J. ZEB2 drives immature T-cell lymphoblastic leukaemia development via enhanced tumour-initiating potential and IL-7 receptor signalling. Nature communications. 2015 Jan 7;6(1):1-2. Epub 2015/01/08. doi: 10.1038/ncomms6794. PubMed PMID: 25565005; PubMed Central PMCID: PMC4354161.
- Simon G, Illyes G, Csiky B. Structural vascular changes in hypertension: role of angiotensin II, dietary sodium supplementation, blood pressure, and time. Hypertension. 1998 Oct;32(4):654-60. Epub 1998/10/17. PubMed PMID: 9774359.
- Clark MS, Rubenach S, Winsor A. A randomized controlled trial of an education and counselling intervention for families after stroke. Clinical Rehabilitation. 2003 Nov;17(7):703-12.
- Shyu YI, Kuo LM, Chen MC, Chen ST. A clinical trial of an individualised intervention programme for family caregivers of older stroke victims in Taiwan. Journal of clinical nursing. 2010 Jun;19(11‐12):1675-85.
- Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, Donaldson N. Training carers of stroke patients: randomised controlled trial. Bmj. 2004 May 6;328(7448):1099.
- Oupra R, Griffiths R, Pryor J, Mott S. Effectiveness of Supportive Educative Learning programme on the level of strain experienced by caregivers of stroke patients in Thailand. Health & social care in the community. 2010 Jan;18(1):10-20.
- G Grant JS, Elliott TR, Weaver M, Bartolucci AA, Giger JN. Telephone intervention with family caregivers of stroke survivors after rehabilitation. Stroke. 2002 Aug 1;33(8):2060-5.
- Mant J, Carter J, Wade DT, Winner S. Family support for stroke: a randomised controlled trial. The Lancet. 2000 Sep 2;356(9232):808-13.
- Mant J, Winner S, Roche J, Wade DT. Family support for stroke: one year follow up of a randomised controlled trial. Journal of Neurology, Neurosurgery & Psychiatry. 2005 Jul 1;76(7):1006-8.
- Van Der Gaag A, Smith L, Davis S, Moss B, Cornelius V, Laing S, Mowles C. Therapy and support services for people with long-term stroke and aphasia and their relatives: a six-month follow-up study. Clinical rehabilitation. 2005 Jun;19(4):372-80.
- Maeshima S, Ueyoshi A, Osawa A, Ishida K, Kunimoto K, Shimamoto Y, Matsumoto T, Yoshida M. Mobility and muscle strength contralateral to hemiplegia from stroke: benefit from self-training with family support. American journal of physical medicine & rehabilitation. 2003 Jun 1;82(6):456-62.
- Fitch M. Providing supportive care for individuals living with cancer. Toronto, ON: Ontario Cancer Treatment and Research Foundation. 1994.
- Tsouna-Hadjis E, Vemmos KN, Zakopoulos N, Stamatelopoulos S. First-stroke recovery process: the role of family social support. Archives of physical medicine and rehabilitation. 2000 Jul 1;81(7):881-7.
- Aguirrezabal A, Duarte E, Rueda N, Cervantes C, Marco E, Escalada F. Effects of information and training provision in satisfaction of patients and carers in stroke rehabilitation. NeuroRehabilitation. 2013 Jan 1;33(4):639-47.
- Shelton W, Moore CD, Socaris S, Gao J, Dowling J. The effect of a family support intervention on family satisfaction, length-of-stay, and cost of care in the intensive care unit. Critical care medicine. 2010 May 1;38(5):1315-20.
- Curzon LB. Teaching in Further Education: an outline of principles and practice. Adolescence. 1998;33(132):957.
- Evans RL, Bishop DS, Haselkorn JK. Factors predicting satisfactory home care after stroke. Archives of Physical Medicine and Rehabilitation. 1991 Feb 1;72(2):144-7.
- Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability?. International disability studies. 1988 Jan 1;10(2):64-7.
- Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of behavioral medicine. 2006 Aug 1;29(4):377-87.
- Lui MH, Mackenzie AE. Chinese elderly patients’ perceptions of their rehabilitation needs following a stroke. Journal of advanced nursing. 1999 Aug;30(2):391-400.
Contact SPER Publications
SPER Publications and
Solutions Pvt. Ltd.
HD - 236,
Near The Shri Ram Millenium School,
Sector 135,
Noida-Greater Noida Expressway,
Noida-201301 [Delhi-NCR] India
